Thanks to your actions, the office of the Ministry of the Attorney General met with the Ontario Working Group on January 15, 2013, to discuss desperately needed prosecutorial guidelines. Crown counsel does not have to prosecute people who use condoms or have a low viral load, just because they can.
US: President’s AIDS council calls on feds to help states repeal HIV criminalisation laws
Advisory group says these statutes are ‘unjust’ and fuel the epidemic
BY TODD HEYWOOD, AMERICAN INDEPENDENT
The Presidential Advisory Council on HIV/AIDS (PACHA) passed a resolution last week that calls for an end to federal and state HIV-specific criminal laws and prosecutions.
While the resolution is only advisory, it recommends that the departments of Justice and Health and Human Services issue guidance and offer incentives to state attorneys general and state health departments to eliminate HIV-specific laws. The advisory group also asks these federal agencies to develop guidelines for how to approach HIV within criminal and civil justice systems that are “consistent with the treatment of similar health and safety risks.”
As the resolution notes, 32 states and two territories have laws criminalizing people living with HIV.
In explaining the reason to repeal these laws, the resolution reads:
People living with HIV have been charged under aggravated assault, attempted murder, and even bioterrorism statutes, and they face more severe penalties because law enforcement, prosecutors, courts, and legislators continue to view and characterize people living with HIV and their bodily fluids as inherently dangerous, even as ‘deadly weapons. Punishments imposed for non-disclosure of HIV status, exposure, or HIV transmission are grossly out of proportion to the actual harm inflicted and reinforce the fear and stigma associated with HIV. Public health leaders and global policy makers agree that HIV criminalization is unjust, bad public health policy and is fueling the epidemic rather than reducing it.
PACHA is also requesting that state and federal authorities review the cases of persons convicted under such laws and overturn convictions if deemed appropriate. The group is calling on the Centers for Disease Control and Prevention to “issue a clear statement addressing the growing evidence that HIV criminalization and punishments are counterproductive and undermine current HIV testing and prevention priorities.”
“Today’s announcement is an important advancement in our collective effort to modernize unjust and discriminatory HIV criminalization laws,” said Rep. Barbara Lee (D-Calif.), co-chair of the Congressional HIV/AIDS Caucus in a statement last week. Lee introduced the REPEAL HIV Discrimination Act in 2011, which never passed, and served on the United Nations’ Global Commission on HIV and the Law.
“I join the President’s Advisory Council on AIDS in calling on the Department of Justice and the Centers of Disease Control and Prevention to issue clear guidance to states and public health departments on the counterproductive effects of HIV criminalization policies; we must end this clear discrimination against people living with HIV,” Lee continued. “Criminalization laws breed fear, discrimination, distrust and hatred, and we must end them.”
The White House declined to comment on the resolution, but the National HIV/AIDS Strategy adopted by the Obama administration in July 2010 does call for state legislatures to “consider reviewing HIV-specific criminal statutes to ensure that they are consistent with current knowledge of HIV transmission and support public health approaches to preventing and treating HIV.”
Policymakers at the state level also welcomed the resolution. Randy Mayer, chief of the Bureau of HIV, STD, and Hepatitis for the Iowa Department of Public Health, said the resolution was a new tool in advocates’ fight to repeal Iowa’s HIV-specific law.
“This resolution came at an excellent time for Iowa,” Mayer said in an email to The American Independent.
State activists and public health officials, including Mayer, have laid out a strategy to repeal the state’s law.
“The advocates in Iowa have also aligned their efforts with a public health perspective, so the resolution was a reinforcement of their justification,” Mayer said. “I think the more public health entities that weigh in on this discussion the better.”
But while policymakers praise the resolution, activists urge cautious optimism.
Sean Strub, executive director of the anti-HIV-criminalization organization Sero Project, said the resolution was appreciated, but the “real test will be in whether federal agencies and the administration responds with the necessary urgency.”
Catherine Hanssens, executive director of the Center for HIV Law and Policy, which runs the Positive Justice Project, echoed Strub’s sentiment, noting that while the resolution is important, PACHA “has no power to order anyone to do anything.”
“[HHS] Secretary [Kathleen] Sebelius and President Obama both have the discretion to ignore the resolution’s recommendations.”
Regardless, Hanssens said the resolution is an important milestone in the battle to repeal HIV criminal laws in the U.S.
“The work of advocates who pushed for passage of the resolution is not over,” she said. “But we have passed a major marker on the road to reform, and justice, for many people and communities affected by HIV.”
UK: Updated guidance on HIV transmission, the law and the work of the clinical team now published
The British HIV Association (BHIVA) and the British Association for Sexual Health and HIV (BASHH) have produced updated guidance on HIV Transmission, the Law and the Work of the Clinical Team.
This guidance is aimed at those working in the field of HIV medicine, especially clinicians, but will also be of use to general practitioners and people living with HIV who want to understand the legal and medical basis for some of their care decisions.
The guidance begins with a clear statement against HIV criminalisation:
BHIVA and BASHH believe that this use of the law is unhelpful and potentially harmful to public health and support UNAIDS recommendations to limit the use of criminal law and the Oslo declaration view that a “non-punitive, non-criminal HIV prevention approach” is preferable.
Covering the law in England & Wales as well as Scotland, the document aims to provide information and guidance on managing issues related to sexual transmission of HIV based on current scientific evidence. It applies generic ethical and professional principles but with a greater emphasis on providing a confidential environment in which extremely sensitive matters can be frankly and fully discussed. This enables appropriate care of people with HIV and benefits public health by encouraging individuals to access testing and treatment. Within this framework this document sets out the roles and responsibilities of health care professionals when caring for individuals living with HIV.
Consistent with the recent BHIVA and the Expert Advisory Group on AIDS (EAGA) position statement on the use of antiretroviral therapy to reduce HIV transmission, the guidance notes:
In most situations the appropriate use of antiretroviral treatment is at least as effective as condoms in preventing sexual transmission of HIV. This is accepted by the [Crown Prosecution Service of England and Wales] and [Scottish Crown Office and Procurator Fiscal Service] so it is likely that evidence showing that the defendant was taking effective antiretroviral treatment at the time of the alleged transmission may be used to demonstrate that they were not reckless.
The guidance also clearly states that healthcare professionals “must be mindful of their duty not to work beyond their expertise in legal matters. For people with HIV, advice must include the routes of HIV transmission and how to prevent transmission, with information about safer sexual practices, the use of condoms and suppression of viral load. Advice must be given in a non-judgmental way.”
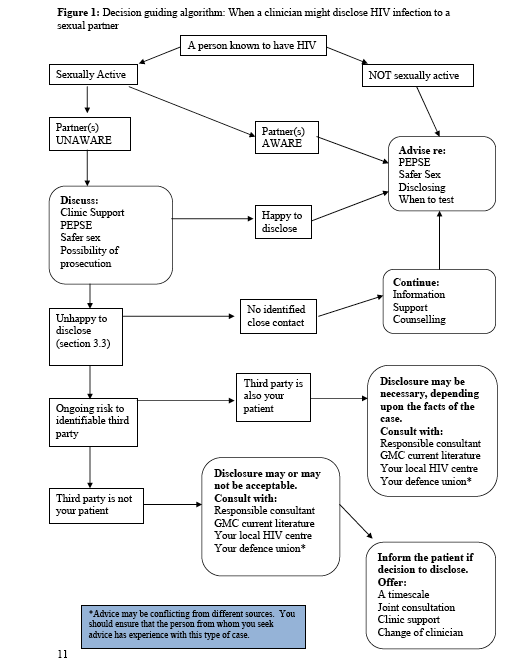
It also discusses issues of confidentiality, noting that “it is important when considering breaching confidentiality to weigh up all potential harms as there may be situations where disclosure of HIV status to protect a sexual partner results in considerable harm to an individual e.g. domestic violence. In situations where a health care professional believes that an HIV positive individual continues to put sexual contacts at risk their duties and subsequent action depend upon the type of contact.” See Figure 1 below.
The guidance also clearly states that “no information should be released to the police unless patient consent has been verified or there is a court order in place, except in very limited circumstances defined by the [General Medical Council].”
Importantly, it also notes that only individuals can make complainants to the police “and health care workers should remain impartial during discussions with patients.”
Finally, it provides clear advice to both help prevent transmission of HIV to sexual partners and to avoid prosecution for ‘reckless’ HIV transmission. Accordingly, people with HIV should do at least one of the following:
- Use a male or female condom fitted correctly along with water-based lubricant. Individuals doing this are unlikely to be seen as reckless for legal purposes. In the event of a condom split, it is advisable to disclose HIV status in order to support the partner’s decision whether or not to obtain post-exposure prophylaxis (PEPSE), which should be taken within 72 hours. The need for PEPSE will depend upon the type of sexual activity and the HIV viral load. An assessment of the risk should be undertaken by a clinician according to the BASHH PEPSE guidelines. Disclosure in these situations would suggest that the person with HIV was not reckless.
- Adhere to effective (suppressed viral load) antiretroviral medication. There is growing evidence of extremely low/minimal risk of transmission when plasma HIV is fully suppressed with the use of antiretroviral medication. In some situations an undetectable viral load can afford protection equivalent to or greater than that of condoms. A person with HIV is unlikely to be seen as reckless when relying on a suppressed viral load instead of condom use if they have been counselled accordingly by an HIV clinician or similar medical authority. It is recommended that this discussion is documented in the patient’s medical records.
In addition people with HIV should be advised that disclosure of HIV positive status to a partner before sex is important to support informed agreement around risk and safer sex behaviours. To avoid successful prosecution an individual who is not taking effective antiretroviral medication and does not use a condom must disclose their HIV status to sexual partners before sex takes place.
The entire guidance is reproduced below.
President's Advisory Council on AIDS (PACHA) approves resolution calling for federal action against HIV criminalization
by Catherine Hanssens Executive Director, CHLP The President’s Advisory Council on AIDS today voted to approve a resolution calling for federal action against HIV criminalization. The resolution includes the following recommendations: 1.
The Register's Editorial: It's time to rethink Iowa's HIV sex law
When you look at the size of the Iowa Code, it’s obvious state officials excel at creating new laws. They are champing at the bit to add more this legislative session. If their goal is really to make Iowa a better place to live, our elected officials should muster as much enthusiasm for repealing problematic statutes.
Des Moines Democratic Senator Matt McCoy wants to change Iowa's HIV disclosure law
DES MOINES, Iowa (AP) – A Des Moines lawmaker plans to introduce legislation that would reduce penalties for HIV-positive people who have sex without disclosing their health condition. Des Moines Democratic Sen. Matt McCoy says he wants to change the law to reduce penalties and focus on people who purposefully infect others with the virus.Under the current law, HIV-positive people who have sex without disclosing their condition can face up to 25 years in prison if convicted, regardless of whether someone is infected. “That is truly a Draconian punishment,” McCoy said. “Being diagnosed with HIV is no longer the death sentence it once was.”
McCoy wants to change the law so someone convicted of intentional or attempted transmission of the virus could be sentenced to a maximum of five years in prison and face a $750 to $7,500 fine. That would put HIV in the same criminal category as transmitting any other communicable disease, such as Hepatitis C. McCoy also wants to end a requirement that people convicted must be placed on a sex offender registry for life.
The Legislature unanimously approved the current law in 1998. The law was approved, in part, as a reaction to a 1996 case in New York where a man intentionally infected 13 women and girls with HIV. Among those voting for the Iowa law was McCoy, who is openly gay. McCoy said the current law made sense based on what was known about HIV and AIDS, but times have changed. “The fact that I’m gay has a real impact on my sensitivity to this issue,” McCoy said. “Clearly, I’m extremely impacted by the gay community and sensitive to people living with HIV. “I just feel it’s the right thing to do for this group of people that have been so stigmatized.”
The proposed changes to the law would take into account whether an HIV-positive person took steps to prevent transmission of the disease, such as using a condom and taking medication that makes it less likely that a sexual partner would be infected. Medications have dramatically improved over the decades, and with proper treatment HIV-positive people can greatly reduce the amount of virus in their blood and make transmission of the disease unlikely.
Randy Mayer, who heads an Iowa Department of Public Health bureau that oversees HIV, said the best way officials can reduce the spread of HIV is to encourage partners to disclose their HIV status to each other. That’s why he agrees with McCoy that the law should be changed. “The law was originally set up to encourage disclosure, but it’s doing the opposite,” he said. “The law is frequently cited by people we work with as something that creates stigma and distrust of the system. … It’s what’s creating stigma.”
McCoy has previously tried to change the law but his bills have become stuck in committees. This time, he said he has support from health care professionals, HIV/AIDS advocacy groups, law enforcement and the Iowa attorney general’s office. Since the Legislature approved the Iowa law, 25 people have been convicted, though only two of those infected partners with HIV. Of those 25, 12 people remain in prison, four are on parole, one is on probation and a trial for one person is pending.
Tami Haught, who became HIV-positive 19 years ago after being infected by her husband, said she supports McCoy’s proposal. Haught works with Community HIV/Hepatitis Advocates of Iowa, which helped draft McCoy’s bill. Haught’s husband became infected through a blood transfusion in the 1980s and died of AIDS in 1996. They married after he was infected. “It takes two people to talk about protection and disclosure. I never had the discussion with my fiance,” she said. “That’s why I hate this law because it puts the entire burden on the HIV person.”
British Columbia's Emergency Intervention Disclosure Act to allow court-ordered HIV testing of anyone who exposes their "bodily substance" to first responders
The Emergency Intervention Disclosure Act was passed on May 31, 2012 and will come into play March 2, 2013. The new regulation sets out the legal and procedural details that support the act, including adding victims of crime to those who can apply for a testing order.
First responders are pleased that in just a month, they’ll have more peace of mind about being exposed to open wounds and needles on the job. In the past victim’s haven’t had to give a blood sample, but now paramedics and firefighters can get a court order. Before this, first responders would often go months wondering if they had contracted a disease like HIV or Hepatitis.
UN Commission on the Status of Women Accepts Statement on HIV Criminalization and Women
The 57th Session of the UN Commission on the Status of Women accepted for publication a Statement calling for the repeal of all laws criminalizing HIV transmission, exposure to HIV, or failure to disclose HIV status.
Washington state plans to amend HIV-specific statute to cover all serious communicable diseases
A Washington state law that criminalizes intentionally infecting other persons with HIV without their consent may be expanded to include any disease that is dangerous or deadly.
New Code for Crown Prosecutors suggests adverse impact on complainant's health may make a prosecution less likely
28/01/2013 The Director of Public Prosecutions, Keir Starmer, QC, has today published a new edition of the Code for Crown Prosecutors, the overarching document that guides prosecutors and police in deciding whether or not to charge a suspect. The publication follows a three month public consultation on a shorter, streamlined version of the Code.