Abstract
Ekubu, Y. (2016) Reducing Vulnerabilities to HIV: Does the Criminalization of HIVAIDS Patients Contribute?. Beijing Law Review, 7, 292-313. doi: 10.4236/blr.2016.74027.
Abstract
Ekubu, Y. (2016) Reducing Vulnerabilities to HIV: Does the Criminalization of HIVAIDS Patients Contribute?. Beijing Law Review, 7, 292-313. doi: 10.4236/blr.2016.74027.
In this article, authors Sienna Baskin, Aziza Ahmed, and Anna Forbes examine the interlocking webs of anti-prostitution laws and HIV criminalisation. Throughout the piece, the authors demonstrate critical research ethics by taking, as their starting point, the lives, freedom, and dignity of sex workers living with HIV.
Baskin et al. describe the ways in which, for sex workers, criminalisation is about so much more than the simple existence of laws. Instead, it is the particular policing and prosecutorial practices in a jurisdiction, based on the laws in place, that shape the lives of sex workers.
Similar to HIV-specific criminal laws, laws criminalising sex work are generally broadly written and arbitrarily enforced, enabling systemic discrimination and bias to turn into prosecutions of people of color and poor people.
The authors detail the consequences of arrest and prosecution that are frequently ignored in discussions of the criminal laws, including violence at the hands of police and fellow inmates, costly fees, possible loss of custody of one’s children, loss of employment and housing, and even loss of the right to sue police for violence that the police enact against sex workers in custody.
When HIV ‘exposure’ is also a crime in a state, then the legal penalties for sex work become even more harmful. If a sex worker is living with HIV, then she or he more often faces a felony rather than misdemeanor charge.
Using public health law mapping, the authors examine the US states that have HIV-specific criminal laws, laws criminalising sex work while living with HIV, and court-imposed mandatory HIV testing for people accused or convicted of sex work.
Baskin et al. find tremendous variety in the legislation from differences in when and how mandatory testing is conducted, to whom HIV test results are revealed, to how the results are used in court.
Of the approximately 32 U.S. states that criminalise HIV ‘exposure’, 14 have specific penalties for HIV-positive sex workers. Eleven states require mandatory HIV testing of sex workers and have enhanced sex work penalties for those living with HIV. Further, those prosecuted for sex work while living with HIV can be prosecuted under general (non HIV-specific) laws in any state.
To be prosecuted in eight states, sexual contact need never occur. People need only to be considered to be “loitering” or to make an offer for sexual services. In ten states, laws mandate testing of those prosecuted for sex work and provide enhanced penalties for those who engage in sex work who are living with HIV. In these states, any arrest after the first arrest (and related mandatory testing) leads to an almost automatic conviction. The HIV testing results become part of the person’s court files.
Noting that, 30 years into the HIV epidemic, there is no evidence that criminal law approaches have any positive effect on HIV prevention, the authors contend that criminalising sex work serves only to harm and discriminate against vulnerable populations and to perpetuate the HIV epidemic.
Details
An article reviewing 15 years of U.S.-based social science research on HIV criminalisation was published in the September 2016 issue of AIDS and Behavior. The research team, led by Dini Harsono of Yale University’s Center for Interdisciplinary Research on AIDS (CIRA), Criminalization of HIV Exposure Work Group, described results from twenty-five research studies conducted in the US from 1990-2014. Studies were conducted with women and men living with HIV, gay men and other men who have sex with men (HIV-positive and –negative), public health workers, and medical providers.
Across the studies, the authors found that, while awareness of HIV exposure laws was generally low, attitudes were generally supportive of criminalisation.[1] The studies showed little to no relationship between the existence of laws and decisions to disclose one’s positive HIV status or to test for HIV. The clearest relationships between stigma and HIV non-disclosure laws could be found from the Sero Project study findings that people living with HIV expect to be treated with bias in the courts simply because of their HIV status. The authors call for future studies to pay more attention to health outcomes, rather than attitudes, and to more closely research prosecution and enforcement practices.
For a global overview of HIV criminalisation research, see O’Byrne et al. (2013). “HIV criminal prosecutions and public health: an examination of the empirical research.”
Criminalization of HIV Exposure: A Review of Empirical Studies in the United States, by Dini Harsono, Carol L. Galletly, Elaine O’Keefe, Zita Lazzarini. AIDS Behavior. DOI 10.1007/s10461-016-1540-5. Published online: 7 Sept 2016.
[1] Although the Sero Project study (2012) was included in the research review, one key set of findings was not discussed. In the Sero Project study, support for criminalisation dramatically declined when survey respondents were provided additional response options (beyond only the choice to support criminalization or not) in survey questions.
Criminalization of HIV Exposure: A Review of Empirical Studies in the United States
(For Russian version, please, scroll down)
At the beginning of 2016, a military officer from Moscow discovered that he was HIV-positive during routine testing. Later, his wife Natalia, who had tested positive for HIV several years ago, admitted that she had been afraid to disclose her HIV-positive status because she feared violent reprisals from her husband. The officer went to the police to commence criminal proceedings against Natalia, and the investigation continues. The media – as in most countries, our only source of information on cases like this – has not yet provided much more information about the case, so we do not know how long Natalia was forced to hide her HIV-positive status from her husband because of fear of violence.
This is not the only case started against a woman for alleged HIV transmission in 2016.
In January, 24-year-old Nadezhda, who lives in the Amur Oblast in the Russian Far East, was found guilty of charges of alleged HIV transmission to three men, under part 1, Art. 122, and part 3, Art. 122 of the Criminal Code (‘infecting others with HIV, knowing about the presence of this disease). She was sentenced to four years in a penal colony. Nadezhda appealed the verdict, but the panel of judges upheld both the verdict and her sentence.
More recently, in the summer of 2016, a 33-year-old woman from Bryansk, 379 kilometers southwest of Moscow, was prosecuted for allegedly infecting her male partner with HIV. The court used evidence that she was registered at an AIDS centre since 2007 against her, since she met the man in 2014. However, the court was relatively lenient, and she was given a three year suspended sentence followed by a three year probation period. In addition, consistent with best practice, her name was not disclosed in the media, in contrast to Nadezhda’s whose name was published in the news release by the Press Service of the Prosecutor’s Office.
At AIDS 2016 in Durban last month, the HIV Justice Network revealed new data showing that Russia now tops the global HIV criminalisation league table. We found reports of at least 115 arrests, prosecutions and/or convictions in Russia during the 30-month period: April 2013 to October 2015.
We have now collected eleven stories from the Russian media about women convicted under Article 122.
Since 2007, at least three of these women were sentenced to more than four years in prison for alleged HIV transmission to one or more partners. Another woman received a sentence of one year, seven months in prison, and a further two women had a suspended one-year and three-year sentence. In one case the court gave a 20 year-old woman 6-month’s probation. Verdicts for three cases are unknown.
It not just alleged HIV transmission that is being prosecuted; we also know of a 2013 case of a woman from the town of Kungur in the Perm Oblast, who was sentenced to spend one year and three months in a penal colony for potential or perceived HIV exposure: her partner was not infected.
Of particular concern is that in all of the above cases, evidence of prior knowledge of HIV-positive status came from medical records. In Russia, each newly-diagnosed person must sign an informed consent form indicating that he or she is informed of their potential criminal liability under Article 122 for HIV exposure and transmission. This informed consent is attached to their medical history, ready for an official request.
Furthermore, in cases of alleged HIV transmission, the public prosecutor did not adequately investigate the causal link between the accused and the complainant, because there is no test that can establish the timing and direction of transmission without any doubt. It is possible, for example, that some of the male complainants were infected before they had relationships with their female partners and before they themselves were diagnosed HIV-positive.
Article 122 was introduced into the Criminal Code, in particular, to protect women from HIV infection, but it is clear from our research that the law has been applied against women in Russia.
There are many reasons why women are vulnerable when HIV criminalisation intersects with gender inequality and violence. These include, but are not limited to, the following:
There is a hope that shedding light on what is going on in Russia will help mobilize people around these unjust prosecutions. As new cases emerge we will continue to report on them on the HIV Justice Network website.
Evgenia Maron is the HIV Justice Network’s EECA Consultant
Presenters: Sean Strub and Dr. Rosita Thomas
A new report released today shows that HIV criminalisation is a growing, global phenomenon. However, advocates around the world are working hard to ensure that the criminal law’s approach to people living with HIV fits with up-to-date science, as well as key legal and human rights principles.
Click on this link to read or download Advancing HIV Justice 2: Building momentum in global advocacy against HIV criminalisation.
What do we mean by ‘HIV criminalisation’?
HIV criminalisation describes the unjust application of the criminal law to people living with HIV based solely on their HIV status – either via HIV-specific criminal statutes, or by applying general criminal laws that allow for prosecution of unintentional HIV transmission, potential or perceived exposure to HIV where HIV was not transmitted, and/or non-disclosure of known HIV-positive status.
Such unjust application of the criminal law in relation to HIV is (i) not guided by the best available scientific and medical evidence relating to HIV, (ii) fails to uphold the principles of legal and judicial fairness (including key criminal law principles of legality, foreseeability, intent, causality, proportionality and proof), and (iii) infringes upon the human rights of those involved in criminal law cases.
What is the impact of HIV criminalisation?
Understanding the potential negative impact of HIV criminalisation on public health is critical to making informed policy decisions.
The last few years have seen increasing interest among researchers in the area of HIV criminalisation and a push into new areas of enquiry to examine the impacts of the unjust application of criminal law.
The report summarises a body of research which shows that instead of delivering a public health benefit, HIV criminalisation is a poor public health strategy, exacerbating racial and gender inequalities and negatively impacting a number of key areas including: testing; disclosure; sexual behaviour; and healthcare practice.
How many countries around the world have HIV criminalisation laws?
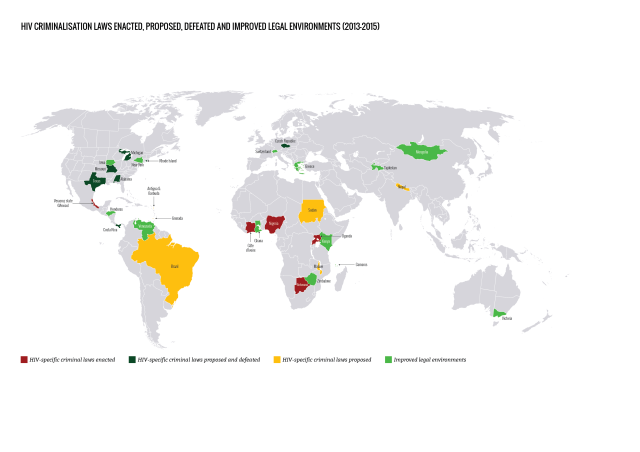
Since our last report, we found an increase in the number of countries that specifically allow for HIV criminalisation: these could be stand-alone HIV-specific criminal laws, part of omnibus HIV laws, or criminal and/or public health laws that specifically mention HIV.
Some of this increase is due to laws enacted since 2013 in Botswana, Cote d’lvoire, Nigeria, Uganda and Veracruz state (Mexico), and some is due to improved reporting and research methodology.
Our analysis shows that a total of 72 countries have adopted laws that specifically allow for HIV criminalisation, either because the law is HIV-specific, or because it names HIV as one (or more) of the diseases covered by the law. This total increases to 101 jurisdictions when the HIV criminalisation laws in 30 of the states that make up the United States are counted individually.

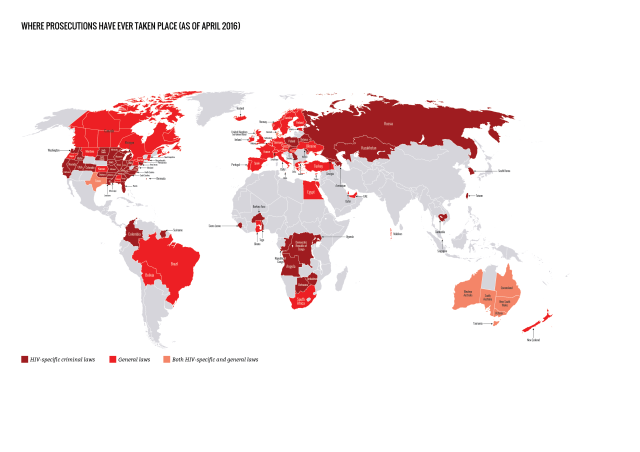
How many countries have prosecuted people living with HIV?
Prosecutions for HIV non-disclosure, potential or perceived exposure and/or unintentional transmission have now been reported in 61 countries. This total increases to 105 jurisdictions when individual US states and Australian states / territories are counted separately.
Of the 61 countries, 26 applied HIV criminalisation laws, 32 applied general criminal or public health laws, and three (Australia, Denmark and United States) applied both HIV criminalisation and general laws.
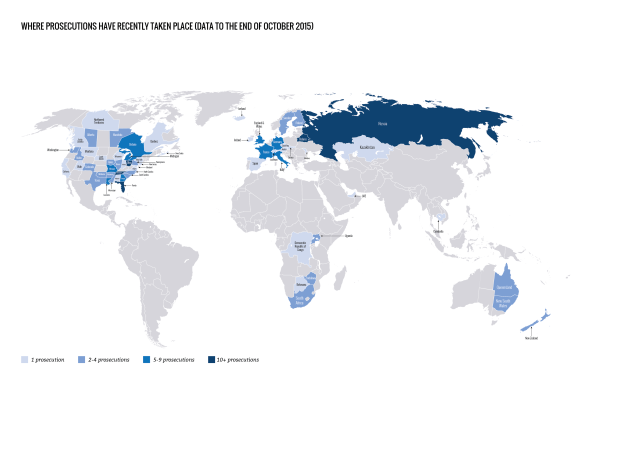
Where have prosecutions recently taken place?
We found reports of at least 313 arrests, prosecutions and/or convictions in 28 countries during the report period, covering 1 April 2013 to 30 September 2015.
Of note, we are now able to include data on reported prosecutions in Belarus and Russia, which are likely to have been taking place at least since the enactment of a Belarusian public health law in 1993 and a Russian HIV criminalisation law in 1995.
The highest number of cases during this period were reported in:
• Russia (at least 115) • United States (at least 104) • Belarus (at least 20) • Canada (at least 17) • France (at least 7) • United Kingdom (at least 6) • Italy (at least 6) • Australia (at least 5) • Germany (at least 5).
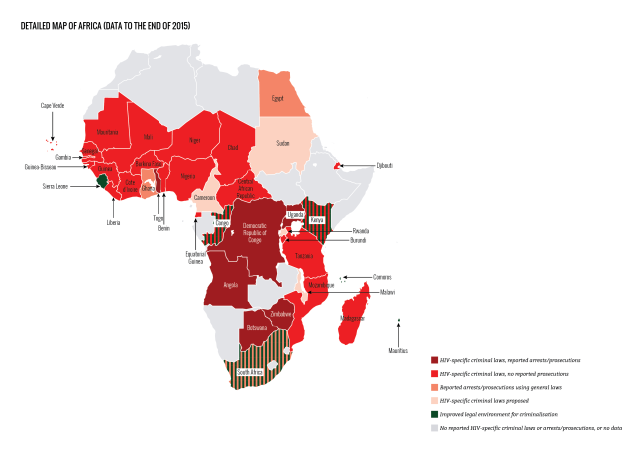
HIV criminalisation in sub-Sarahan Africa of increasing concern
Where there was no HIV criminalisation at the start of the 21st century, 30 sub-Saharan African countries have now enacted overly broad and/or vague HIV-specific criminal statutes.
Most of these statutes are part of omnibus HIV-specific laws that also include protective provisions, such as those relating to non-discrimination in employment, health and housing. However, they also include a number of problematic provisions such as compulsory HIV testing and involuntary partner notification, as well as HIV criminalisation.
During the period covered by this report four countries in sub-Saharan Africa passed new HIV criminalisation laws: Botswana, Cote d’lvoire, Nigeria and Uganda.
Very few countries in Africa are now unaffected by problematic HIV criminalisation laws. The rise of reported prosecutions in Africa during this period (in Botswana, South Africa, Uganda, and especially Zimbabwe), along with the continuing, growing number of HIV criminalisation laws on this continent, is especially alarming.
Where has advocacy improved legal environments?
Important and promising developments in case law, law reform and policy have taken place in many jurisdictions, most of which came about as a direct result of advocacy.
During the report period, although an additional 13 jurisdictions in nine countries proposed new HIV criminalisation laws, seven of these were not passed, primarily due to swift and effective advocacy against them at an early stage. Advocacy in another ten jurisdictions in seven countries challenged, improved or repealed HIV criminalisation laws.
The legal environment relating to HIV criminalisation has improved in a small number of countries in sub-Saharan Africa, most notably in Kenya. On 18 March 2015, Kenya’s High Court ruled that its HIV criminalisation provision – Section 24 of the HIV Prevention and Control Act 2006 – was unconstitutional because it was vague, overbroad and lacking in legal certainty, particularly in respect to the term ‘sexual contact’.
The Court also found it contravened Article 31 of the Kenyan Constitution which guarantees the right to privacy because the law created an obligation for people with HIV to disclose their status to their ‘sexual contacts’, with no corresponding obligation for recipients of such sensitive medical information to keep it confidential.
Using science as an advocacy tool
Increased knowledge about reduced infectiousness due to antiretroviral therapy has led to advocacy that resulted in a number of jurisdictions revising or revisiting their criminal laws or prosecutorial policies relating to HIV criminalisation, although progress has been frustratingly slow.
Following the ‘Swiss statement’, published in January 2008, a growing number of courts, government ministries and prosecutorial authorities have accepted antiretroviral therapy’s impact on reducing the risk of both HIV exposure and transmission.
However, scientific advances alone will neither ‘end AIDS’ nor end HIV criminalisation. Although the impact of antiretroviral therapy on infectiousness is an important advocacy tool, it must be remembered that many people with HIV do not have access to treatment (or are unable to achieve an undetectable viral load when on treatment) and that everyone has a right to choose not to know their status and/or start treatment and should not be stigmatised nor considered ‘second class citizens’ should they wish to delay diagnosis or antiretroviral therapy.
More work required
Despite the many incremental successes of the past few years, much more work is required to strengthen advocacy capacity. This is why a coalition of seven organisations launched HIV Justice Worldwide in April 2016.
We also need to be aware that HIV criminalisation does not exist in vacuum, and is often linked to punitive laws and policies that impact sexual and reproductive health and rights, especially those aimed at sex workers and/or men who have sex with men and other sexual minorities.
And, bearing in mind the stigma faced by those with, for example, hepatitis C and concerns over the sexual transmission of the Ebola and Zika viruses, as we move forward to eliminate – or modernise – HIV criminalisation laws, we must ensure that our work does not inadvertently lead to the further criminalisation of other communicable and/or sexually transmitted infections.
Click on this link to read or download Advancing HIV Justice 2: Building momentum in global advocacy against HIV criminalisation.
A note about the limitations of the data
The data and case analyses in this report covers a 30-month period, 1 April 2013 to 30 September 2015. This begins where the original Advancing HIV Justice report – which covered the 18-month period, 1 September 2011 to 31 March 2013 – left off. Our data should be seen as an illustration of what may be a more widespread, but generally undocumented, use of the criminal law against people with HIV.
A year ago, in April 2015, the French National AIDS and Viral Hepatitis Council (Conseil national du sida et des hépatites virales, known simply as ‘CNS’) following extensive research into the law, nature of complaints and prosecutions, and their impact, issued a report, opinion and recommendations.
An English language version of the report, opinion and subsequent recommendations is still being prepared.
Earlier this year, Professor Patrick Yeni (pictured), chair of the CNS, was interviewed by Jean-François Laforgerie on the French language HIV website, seronet.info. His interview is eye-opening and powerful.
It highlights that although they had only found 23 convictions up to the end of 2014, surveys of people living with HIV suggest that up to 2000 complaints may have been made since the start of the epidemic.
The survey shows that slightly more than one person living with HIV in ten claims to have been tempted to complain against the person that they believed to be the source of infection. According to the same source, 1.4% of people living with HIV surveyed reported having actually complained. Based on these figures, we estimate an order of magnitude from 1 500 to 2 000 complaints that could be filed in total since the beginning of the epidemic.
He also notes that the law currently only recognises condom use as a way to show lack of a guilty mind, and he and his colleagues are concerned that up-to-date science is not reflected in the law. He also highlights that in France disclosure of known HIV-positive status – and subsequent consent to ‘risky’ sex – is not actually a defence, although in practice only cases where no disclosure took place and where no condoms were used have reached the court.
It seems unthinkable that what is obvious in terms of public health today on the promotion of biomedical preventions is lagging behind legally.
Given the importance of this body of work, we have decided to publish the interview and a summary of the main CNS recommendations beneath it, despite no official English translation.
It is interesting that the people who complain and go to trial are not part of the so-called risk groups where prevalence is high. For example, there is virtually no migrants among the complainants. Moreover, today there is a much greater legalisation of intimacy, including sexual facts than existed in the past. Perhaps this plays on the fact that people complain more now than twenty years ago.
Below is the English translation of the seronet.info interview, further improved from Google translate’s version by Sylvie Beaumont. Version anglaise via Google translate. Le texte français est après la traduction.
Patrick Yeni [PY]: The media coverage of some trials in France and, secondly, the situation internationally. In other countries, there was an active debate on the criminalisation of HIV transmission, while in France this reflection seemed stalled. These are the two reasons that led us to revisit this issue, trying to understand and think about how things had changed since our first review.
PY: We have no clear answer to that. This is also why we wanted to restart the debate. If one takes the point of view of government and we take stock of court cases – 23 convictions for HIV transmission since the beginning of the epidemic throughout France – one can imagine that for the state this is not a national major problem at the criminal level, at least quantitatively. I guess the debate on criminal justice focuses primarily on other issues. For HIV organisations, it is probably more complicated because legal proceedings – as we attempt to analyse them in the recommendations – somewhat undermined the historical foundations on which the fight against HIV is based. By that I mean solidarity between people living with HIV and the refusal to distinguish between “patients as victims” allegedly infected and others who simply became infected. I imagine that this problem could have induced some inertia in advancing the debate. One recommendation from the CNS is to urge organisations to resume this discussion today, because it is a lever to act on issues of stigma, discrimination … and HIV prevention in general.
PY: Primarily the fact that a person who knows s/he is HIV-positive, transmits HIV to a partner while s/he has not taken preventive measures to prevent this, i.e used a condom. In almost all trials in France, this is what has been prosecuted. We have had discussions on other issues as lawyers who supported us explained that the scope of what could be prosecuted or what could be an offence is probably wider than what is actually applied today.
PY: One must think on several levels. The first criterion is that they are people who know they are HIV-positive. But it’s more complicated. Thus, from a legal point of view, we cannot know that a person, while not knowing officially that they are HIV-positive would consider themselves to be negative while they are engaged in repeated risky sexual behaviour. Justice may consider that even if they did not know their status officially, their sexual behaviour should have pushed them to consider themselves as potentially HIV-positive, and therefore to do a test and take preventive measures. In this case, the absence of screening does not guarantee the absence of criminal risk. The second criterion is that there must be proof that the person has transmitted HIV. Our analysis of judgments shows that exposing someone to HIV transmission, even without actual transmission can also be penalised. There have been convictions in France for exposure to the risk of transmission. This has occurred in the case of additional convictions to convictions for actual transmission, but it exists.
PY: Yes. The legal elements are there. That is, according to our analysis, another possibility of expanding the criminal field. The third criterion is that the ‘victim’ is not aware of the HIV status of their partner. In criminal law, whether or not the victim is informed does not exempt the defendant from liability. One cannot argue that the partner was informed and has agreed not to protect themselves and therefore would not be responsible. The information is not enough.
Fourth criterion. In all cases today, sexual prevention is understood as the use of condoms. It is the condom which is retained as the manifestation of concerns relating to the risk of transmission. We do not know what will happen when there will be proceedings for transmission or exposure by people who do not use condoms, but are treated effectively. Some lawyers have told us that if there was transmission despite condom use, it would be a case of force majeure which is exculpatory of responsibility. We can not guarantee the same thing about treatment. In other words, even with a good track treatment, a viral load of less than 20 copies, one cannot guarantee that there is not occasionally a little HIV in semen … and therefore transmission is possible even if treatment is adhered to, and viral load is undetectable … other lawyers tell us that we are, in this case, in a random situation, which does not exempt the person with HIV from responsibility. We must think about this. It seems unthinkable that what is obvious in terms of public health today on the promotion of biomedical preventions is lagging behind legally. This is a warning that we mention in the recommendation. But unfortunately we fear that this debate will only take place when a case of transmission from someone on effective treatment will come to court.
PY: We wanted to alert on this point precisely so the conclusions of judges, when they have to decide, are identical to the public health conclusions we know today. We must not get to this contradiction where a person who is effectively treated is found guilty because s/he would not use a condom. With these examples, we can see the narrow scope of what is actually prosecuted and that it is imperative to have a debate on the possible expansion of what is a crime.
PY: The review analysed the consequences of the criminalisation of HIV transmission on testing. All the studies to which we had access, mainly foreign, do not indicate that criminal risk linked to knowing one’s status would lead to decreased use of testing.
PY: We had discussions about it. Some of us were reluctant to say that there was an increase in the number of cases. One thing is certain, we are on a low figure: 23 convictions. Especially if we compare the data of the ANRS-Vespa 2 survey. The survey shows that slightly more than one person living with HIV in ten claims to have been tempted to complain against the person that they believed to be the source of infection. According to the same source, 1.4% of people living with HIV surveyed reported having actually complained. Based on these figures, we estimate an order of magnitude from 1,500 to 2,000 complaints that could be filed in total since the beginning of the epidemic. We do not know why some complaints were accepted and others not, why some were eventually classified and others have prospered. We have, unfortunately, no way to evaluate it. We just know that few cases reach a conviction.
To respond more specifically, one must take into account the fact that there is a significant delay, sometimes ten years from the time a complaint is filed to the time when an appeal judgment is pronounced. It might be possible to say that today there is an increase in the number of procedures, but it is not certain. We must be careful about this point. If this is true, how can we explain it? One hypothesis is that in the early days of the epidemic, when many people died of AIDS, a complaint against a person who was likely to die did not make much sense. Today the situation is different. For people, this may appear more “logical” to do so. We advance this hypothesis, but we don’t have the figures to confirm it. One can also look at who is complaining. It is interesting that the people who complain and go to trial are not part of the so-called risk groups where prevalence is high. For example, there is virtually no migrants among the complainants. Moreover, today there is a much greater legalisation of intimacy, including sexual facts than existed in the past. Perhaps this plays on the fact that people complain more now than twenty years ago.
PY: Firstly: to inform people living with HIV about the conditions under which their criminal responsibility may be engaged. Our thinking has focused on being able to contribute to a fair justice. How? By raising awareness of the investigators in this matter through the National Schools of Police and Gendarmerie. By working with judges and lawyers. It is not possible for judges to have the technical knowledge about different diseases, we admit. Similarly, we can not consider today that under the pretext that people no longer die of AIDS, HIV is commonplace. This is not possible even today because there is a context of social representations that make it a special disease. However, the situation is not the same today, in particular medical progress has taken place. It is very important that judges and lawyers are aware of this. We propose that the National School of Magistrates opens this debate in its initial training as well as in continuing education. We asked the school director to include a discussion on HIV in its knowledge training. A problem that does not concern judges, is that of upgrading one’s knowledge to contribute to a fair trial. One of our wishes is also to allow a reflection on the position of criminal justice. Prison sentences predominate in cases of HIV transmission and issues of rehabilitation and prevention of relapses are not taken into account, even though the court must ensure both aspects in its approach.
PY: For the Department of Justice to develop a form of observatory monitoring of judgments, to document the characteristics of procedures. The tool does not exist and we had to carry out considerable work to realise our new advice and to find all cases that resulted in convictions. We must create an interdepartmental committee to work on the development and provision of information tools tailored to professional (police, lawyers, judges) and other persons concerned, so that the procedures take account of available scientific and medical data, and for doctors to be better informed about the criminal risk of HIV transmission. It’s lobbying work which we pursue, including with HIV organisations. They must reclaim this question on which they were at a standby. We must recognise that the right to resort to justice is a right for all citizens, that our struggle is not against criminal law, but rather to ensure a fair process and prevent risks of criminalisation.
Summary of the CNS’s 2015 recommendations on HIV criminalisation
| No. | Objectives | Recommendations | Competent authorities
and/or recommendation targets |
| 1 | Contribute to better information of judges | Promote initial and continuing education of magistrates and future magistrates on HIV related issues | French National School for the Judiciary (école nationale de la magistrature) |
| 2 | Bolster the quality of police investigations | Promote training actions of police officers and future officers on HIV related issues | Ministry of the Interior |
| 3 | Prevent reoffending, enable the integration and reintegration of convicted people and improve their support | Apply alternatives to custodial sentences | Ministry of Justice |
| 4 | Promote the prevention of the prosecution risk | Contribute to a better understanding of legal issues by the people and communities concerned | HIV/AIDS associations |
| Support actions aiming to provide information on the legal rights and responsibilities of people living with HIV. | Ministry of HealthFrench National Institute for Health Prevention and Education (INPES) | ||
| Promote actions to fight PLHIV stigmatisation and discrimination and prevention actions towards the general population | Ministry of Health, Regional Health Agencies (ARS), French National Institute for Health Prevention and Education (INPES)Other competent ministriesHIV/AIDS associations | ||
| 5 | Provide access to up-to-date and high-quality legal and scientific information | Implement a reporting tool to follow-up the rulings issued in France and to document the characteristics of the related proceedings | Ministry of Justice |
| Initiate the creation of a working group in charge of designing and provisioning of information tools suitable for professionals and people involved | Health/Justice Interministerial Committee |
Article original
PÉNALISATION DE LA TRANSMISSION DU VIH : GARANTIR UNE PROCÉDURE ÉQUITABLE
Où en est-on aujourd’hui en France sur la pénalisation de la transmission de VIH ? Le professeur Patrick Yéni, président du Conseil national du sida (CNS) fait le point. Interview.
In 2006, le Conseil national du sida et des hépatites virales (CNS) avait publié un premier avis sur la pénalisation de la transmission du VIH. Qu’est-ce qui vous a conduit à travailler de nouveau sur ce sujet et à publier, en 2015, un second avis ?
Patrick Yeni : Il y a la médiatisation de certains procès en France et, d’autre part, le constat sur le plan international, dans d’autres pays concernés, qu’il y avait une réflexion active sur la pénalisation de la transmission de l’infection par le VIH alors qu’en France cette réflexion semblait marquer le pas. Ce sont ces deux raisons qui nous ont conduits à retravailler sur cette question, en essayant de comprendre et de réfléchir à la façon dont les choses avaient évolué, depuis notre premier avis.
Nous n’avons pas de réponse claire à cela. C’est aussi pour cela que nous avons voulu reprendre cette réflexion. Si l’on se place du point de vue des pouvoirs publics et que l’on fait le bilan des affaires judiciaires — soit 23 condamnations pour transmission du VIH depuis le début de l’épidémie pour toute la France —, on peut imaginer que pour l’Etat il ne s’agit pas là d’un problème majeur national au niveau pénal, du moins sur le plan quantitatif. J’imagine que la réflexion sur la justice pénale porte prioritairement sur d’autres questions. Pour les associations de lutte contre le sida, c’est probablement plus compliqué parce que les procédures judiciaires — comme nous essayons de l’analyser dans l’avis — mettent quelque peu à mal les fondements historiques de la lutte contre le VIH. Je citerai la solidarité entre les personnes atteintes et le refus de distinguer entre des “malades victimes” qui auraient été contaminés et d’autres qui se seraient infectés. J’imagine que cette difficulté a pu introduire de l’inertie dans la progression de la réflexion. C’est justement une recommandation du CNS que d’exhorter les associations à reprendre aujourd’hui cette réflexion, parce qu’elle constitue un bras de levier pour agir sur les stigmatisations, les discriminations… et la prévention en général.
C’est avant tout le fait pour une personne qui se sait séropositive d’avoir transmis le VIH à un ou une partenaire alors qu’elle n’avait pas pris de mesure de prévention pour prévenir cette transmission, en l’occurrence l’utilisation de préservatif. Dans la quasi-totalité des procès en France, c’est cela qui est condamné. Nous avons eu des réflexions sur d’autres points car les juristes qui nous ont accompagnés ont expliqué que le champ de ce qui est condamnable, de ce qui pourrait représenter un délit, est sans doute plus large que celui qui est effectivement appliqué aujourd’hui.
Il faut raisonner sur plusieurs niveaux. Le premier critère retenu est que ce sont des personnes qui se savent séropositives. Mais c’est plus compliqué. Ainsi, d’un point de vue juridique, on ne peut assurer qu’une personne bien que ne se sachant pas formellement séropositive puisse se considérer comme séronégative alors qu’elle est engagée dans des comportements sexuels à risques, répétés. La justice peut considérer que même si elle ne sait pas de façon formelle quel est son statut, son comportement sexuel aurait du l’inciter à se considérer comme potentiellement séropositive, donc à se tester et à mettre en œuvre des moyens de prévention. Dans ce cas, l’absence de dépistage ne garantit pas l’absence de risque pénal. Le deuxième critère est qu’il faut la preuve que la personne ait transmis le VIH. Notre analyse des jugements montre que le fait d’exposer à la transmission du VIH, même sans transmission effective, peut également être pénalisé. Il y a eu des condamnations en France pour exposition au risque de transmission. Cela s’est produit dans des cas de condamnations additionnelles à des condamnations pour transmission effective, mais cela existe.
Oui. Les éléments juridiques sont là. C’est, selon notre analyse, une autre possibilité d’élargissement du champ pénal. Le troisième critère est le fait que la victime ne soit pas informée de la séropositivité du ou de la partenaire. En droit pénal, le fait que la victime soit informée ou pas n’exonère pas le prévenu de sa responsabilité. On ne peut pas arguer que le partenaire était informé et qu’il a accepté de ne pas se protéger et donc qu’on ne serait pas responsable. L’information ne suffit pas.
Quatrième critère. Dans toutes les affaires aujourd’hui, la prévention des rapports sexuels est comprise comme l’usage du préservatif. C’est le préservatif qui est retenu comme la manifestation de la préoccupation face au risque de transmission. Nous ne savons pas ce qui se passera lorsqu’il y aura des procédures engagées pour transmission ou exposition concernant des personnes qui n’utilisent pas de préservatifs, mais qui sont traitées efficacement. Certains juristes nous ont expliqué que s’il y avait transmission malgré l’usage du préservatif, il s’agirait d’un cas de force majeure qui est exonératoire de la responsabilité. On ne peut pas garantir la même chose concernant le traitement. Autrement dit, avec un traitement bien suivi, une charge virale dans le sang inférieure à 20 copies, on ne peut pas garantir qu’il n’y ait pas de temps en temps un peu de VIH dans le sperme… et donc qu’une transmission soit possible même si le traitement est bien suivi, la charge virale indétectable… D’autres juristes nous disent que nous sommes, dans ce cas-là, dans une situation d’aléa, qui, elle, n’est pas exonératoire de la responsabilité. Nous devons réfléchir à cela. Il paraîtrait impensable que ce qui est une évidence en termes de santé publique aujourd’hui sur la promotion des préventions biomédicales, soit en décalage sur le plan juridique. C’est un motif d’alerte que nous mentionnons dans l’avis. Mais il est à craindre malheureusement que cette réflexion n’ait lieu que le jour où un cas de transmission concernant une personne sous traitement efficace vienne au tribunal.
Nous avons souhaité alerter sur ce point afin que justement les conclusions de la justice, lorsqu’elle aura à se prononcer, soient identiques aux conclusions de santé publique que nous connaissons aujourd’hui. Nous ne devons pas arriver à cette contradiction qu’une personne qui se traiterait efficacement soit condamnée parce qu’elle n’utiliserait pas le préservatif. Avec ces exemples, on voit bien l’espace assez restreint de ce qui est effectivement condamné aujourd’hui et le fait qu’il faut absolument avoir une réflexion sur le possible élargissement de ce qui est condamnable.
L’avis a analysé les conséquences de la pénalisation de la transmission en matière de recours au dépistage. Toutes les études auxquelles nous avons eu accès, essentiellement étrangères, n’indiquent pas que le risque pénal lié à la connaissance de son statut sérologique conduirait à une diminution du recours au dépistage.
Nous avons eu des discussions à ce sujet. Certains d’entre nous étaient réticents à affirmer qu’il y avait une augmentation du nombre de cas. Une chose est sûre, nous sommes sur un chiffre bas : 23 condamnations. D’autant plus si on le rapporte aux données de l’enquête ANRS-Vespa 2. L’enquête montre qu’un peu plus d’une personne vivant avec le VIH sur dix déclare avoir été tentée de porter plainte contre la personne qu’elle estimait être à l’origine de sa contamination. Selon la même source, 1,4 % des personnes vivant avec le VIH interrogées déclaraient avoir effectivement porté plainte. Sur la base de ces chiffres, nous avons estimé un ordre de grandeur de 1 500 à 2 000 plaintes qui auraient pu être déposées au total depuis le début de l’épidémie. Nous ne savons pas pourquoi certaines plaintes ont été acceptées et d’autres pas, pourquoi certaines ont finalement été classées et d’autres ont prospéré. Nous n’avons, hélas, aucun moyen d’évaluer cela. Nous savons juste que peu d’affaires arrivent à une condamnation.
Pour répondre plus précisément, il faut prendre en compte le fait qu’il y a un délai important, parfois dix ans, entre le moment où une plainte est déposée et celui où un jugement en appel est prononcé. Dire qu’aujourd’hui nous sommes sur une augmentation du nombre de procédures, c’est possible, mais pas certain. Nous devons être prudents sur ce point. Si c’est vrai, comment l’expliquer ? Une des hypothèses, c’est qu’aux premiers temps de l’épidémie, lorsque beaucoup de monde décédait du sida, porter plainte contre une personne qui allait sans doute mourir n’avait pas grand sens. Aujourd’hui, la situation est différente. Pour des personnes, cela peut apparaître plus “logique” de le faire. Nous avançons cette hypothèse, mais aucun chiffre ne permet de la confirmer. On peut aussi regarder quels sont ceux qui portent plainte. C’est intéressant de voir que les personnes qui portent plainte et arrivent au procès ne font pas partie des groupes dits à risques où la prévalence est très forte. Par exemple, il n’y a quasiment pas de personnes migrantes parmi les plaignants. Par ailleurs, il existe aujourd’hui une judiciarisation bien plus importante de l’intime, notamment des faits sexuels, qu’elle n’existait dans le passé. Peut-être cela joue-t-il dans le fait de porter plainte plus aujourd’hui qu’il y a vingt ans.
Tout d’abord : informer les personnes vivant avec le VIH sur les conditions dans lesquelles leur responsabilité pénale peut être engagée. Notre réflexion a surtout porté sur le fait de pouvoir contribuer à une justice équitable. Par quels moyens ? Par une sensibilisation des enquêteurs à cette question par les écoles nationales de police et de gendarmerie. Par un travail auprès des magistrats et des avocats. Il n’est pas possible que les juges aient des connaissances techniques sur les différentes maladies, nous l’admettons. De la même façon, on ne peut pas considérer aujourd’hui, au prétexte qu’on ne meure plus du sida, que l’infection par le VIH est banale. Ce n’est pas possible parce qu’il existe un contexte de représentations sociales qui en font une maladie particulière. Pour autant, la situation n’est plus la même aujourd’hui, des progrès notamment médicaux ont eu lieu. C’est très important que les magistrats et les avocats aient connaissance de cela. Nous proposons que l’Ecole nationale de la magistrature ouvre cette réflexion dans sa formation initiale, comme dans sa formation continue. Nous avons sollicité le directeur de cette école pour lui demander d’inclure une réflexion autour du VIH dans la formation des connaissances. Un problème, qui ne concerne pas que les juges, est celui de la mise à niveau des connaissances pour contribuer à une justice équitable. Un de nos souhaits est aussi de permettre de réfléchir à la position de la justice pénale. Les peines de prison ferme prédominent dans les affaires de transmission du VIH et les questions de réinsertion et de prévention de la récidive ne sont pas du tout prises en compte, alors même que la justice doit veiller à ces deux aspects dans sa démarche.
Pour le ministère de la Justice, de se doter d’une forme d’observatoire de suivi des jugements rendus, de documenter les caractéristiques des procédures. L’outil n’existe pas et nous avons dû effectuer un travail considérable pour réaliser notre nouvel avis et retrouver tous les cas ayant abouti à des condamnations. Il faut créer un comité interministériel pour qu’il travaille à la création et la mise à disposition d’outils d’information adaptés aux professionnels (policiers, avocats, magistrats) et aux personnes concernées, pour que les procédures tiennent compte des données scientifiques et médicales disponibles, pour que les médecins soient mieux informés sur le risque pénal de la transmission du VIH. C’est du travail de lobbying que nous menons, y compris auprès des associations de lutte contre le sida. Elles doivent se réapproprier cette question, sur laquelle elles étaient un peu en situation de veille. Nous devons admettre que le droit au recours à la justice est un droit des citoyens, que notre combat n’est pas contre la justice pénale, mais plutôt pour garantir une procédure équitable et prévenir le risque pénal.
Propos recueillis par Jean-François Laforgerie.
by Tyler J. Smith
J.D., 2015, Indiana University Robert H. McKinney School of Law
H-I-V. Arguably, no three letters in American society have generated more fear of a “viral underclass” [1] than those associated with the Human Immunodeficiency Virus (“HIV”). In many states, including Indiana, simply having HIV is a crime with potentially severe consequences. The criminalization of HIV is founded on a fear of something many people do not fully understand and the stigma of “HIV’s association with an ‘outlaw’ sexuality, anal intercourse, gay men, people of color, and people who use drugs.” [2] Indeed, convictions under these statutes rarely have anything to do with actual HIV transmission or risk of transmission. [3] Over thirty states currently have HIV specific criminal statutes “based on perceived exposure to HIV, rather than actual transmission of HIV to another.” [4]
The Infectious Diseases Society of America (IDSA) and HIV Medical Association (HIVMA) assert that “[c]riminalization is not an effective strategy for reducing transmission of infectious disease and in fact may paradoxically increase infectious disease transmission.” [5] Studies further indicate that “these laws discourage individuals from being screened and treated for conditions when early diagnosis and treatment of infected individuals is one of the most effective methods to control the disease.” [6] More people have been convicted under these laws in the United States and Canada than all other countries in the world combined. [7]
Numerous examples illustrate the unfounded fear and stigma that fuel egregious convictions and unjust sentences of HIV positive people. An HIV positive man in Michigan was charged under the state’s anti-terrorism statute with possession of a “biological weapon” after he allegedly bit his neighbor. [8] Another HIV positive man in Texas is currently serving thirty-five years for spitting at a police officer. [9] A man in Iowa with an undetectable viral load received a twenty-five year sentence after a one-time sexual encounter in which he wore a condom. [10] His sentence was suspended, but he was placed on probation for five years and had to register as a sex-offender for ten years. [11]
Many states rightfully criminalize reckless, knowing, or intentional behaviors that actually put others at significant risk. However, some states have other criminal statutes that are overbroad, or criminalize simply having HIV and engaging in conduct that scientifically poses no risk of transmission. Such statutes clearly exhibit a complete lack of scientific understanding of how HIV is transmitted and because of their overbroad nature, give prosecutors “significant discretion in determining whether and how to prosecute individuals arrested or reported for HIV exposure.” [12] The actual risk of transmission depends on the amount of the virus in a person’s blood. [13] The risk-per-exposure for various sex acts, without factoring in how condoms or medical treatment reduce the risk even further, ranges from zero to eighty-two in 100,000. [14] Intravenous drug use risk-per-exposure ranges from sixty-three to 240 in 100,000. [15] Despite the relatively low risk, “courts rarely look at what a person did to further reduce the risk of transmission.” [16] Simply having HIV is a considered a crime.
With overwhelming bi-partisan support, criminalization of HIV became federal in 1990 with the Ryan White Comprehensive AIDS Resources Emergency Act. [17] The Act’s namesake, Ryan White, a thirteen-year old boy from Russiaville, Indiana, contracted the disease in 1984 following a blood transfusion. [18] This act created The Ryan White HIV/AIDS Program; the “most comprehensive Federal program that provides services exclusively to people living with HIV.” [19] It serves more than 500,000 people that do not have adequate health care coverage to manage their treatment. [20]
Congress exercised its power to control funding by requiring states to “protect against intentional transmission” to receive federal funding for the new program. [21] Section 2647 of the Act provided in part that “[t]he Secretary may not grant . . . to a State unless the chief executive officer determines that the criminal laws of the State are adequate to prosecute any HIV infected individual” who intended to transmit HIV through donation of bodily fluid, engaging in sexual activity intending to transmit HIV, or shared needles intending to transmit HIV. [22] This provision was repealed in 2000; however, the seeds for states to go above and beyond were already sown. Some states went further than what the federal law required by defining intentional transmission as non-disclosure of their positive status to a sexual partner. [23]
Although thirty-plus states criminalize HIV under HIV-specific criminal statutes or STD criminal statutes that specifically encompass HIV, [24] zero states have criminalized the transmission or the failure to disclose the positive status of other sexually transmitted diseases, such as the Human Papillomavirus (“HPV”). [25] According to the Centers for Disease Control and Prevention (“CDC”), 33,000 new cases of cancer are reported each year with about 26,900 of these cancers caused by HPV. [26] Nearly all cases of cervical cancer are caused by HPV [27] and 4074 women died of cervical cancer in 2012. [28] In 2013, an estimated 9278 women received a new diagnosis of HIV. [29] In 2012, among women who previously received a diagnosis of AIDS, an estimated 3561 women died. [30] Thus, more women were diagnosed with cancer caused by HPV than women who were diagnosed with HIV and more women died of cancer caused by HPV than women who died of AIDS. [31] Yet HPV has not been criminalized in any state. [32]
Portions of Indiana’s criminal code do make sense. Someone who recklessly, knowingly, or intentionally donates or sells semen or blood that contains HIV could rightfully face felony charges. [33] However, other statutory provisions in the criminal code are overbroad and punish scientifically unfounded conduct. For example, a person without HIV can be charged with a Class C Misdemeanor for “battery” by placing bodily fluid or waste on another person in a rude, insolent, or angry manner. [34] A person without HIV can be charged with “malicious mischief,” a Class B Misdemeanor, for placing bodily fluid or fecal waste with the intent that another person will involuntarily touch it. [35] If a person is HIV positive, both of these offenses become Level 6 Felonies for exposing to others any bodily fluid, including those scientifically proven to not transmit HIV. [36] Battery is a Level 5 Felony if the bodily fluid or waste is placed on a public safety officer, but only if the accused is HIV positive. [37] If the accused is not HIV positive, then committing battery on a public safety officer remains a Level 6 Felony. [38] Therefore, simply having HIV statutorily increases the penalty for these offenses.
Despite laws to the contrary, the CDC clearly states that “[c]ontact with saliva, tears, or sweat has never been shown to result in transmission of HIV.” [39] Very low quantities of HIV have been found in the saliva and tears of some AIDS patients. [40] However, “finding a small amount of HIV in a body fluid does not necessarily mean that HIV can be transmitted by that body fluid.” [41] HIV has not been found in the sweat of HIV-infected patients. [42] Indiana prosecutors have discretion to prosecute HIV positive persons criminally for a variety of offenses related to their HIV positive status regardless of intent to transmit or actual transmission and regardless of whether transmission is even scientifically possible.
Indiana law also criminalizes simply having what it defines a “dangerous communicable disease.” [43] Carriers of HIV, AIDS, and Hepatitis B have a duty to “warn or cause to be warned by a third party a person at risk” of the carrier’s disease status and the need to seek healthcare. [44] HIV positive persons must disclose their status to past, present, and future sexual or needle-sharing partners or face criminal penalty. [45] The burden of proof shifts to the accused to show he or she in fact disclosed his or her positive status to those past, present, or potential partners. [46] A person who “recklessly” violates the statutory provision commits a Class B Misdemeanor. [47] A person who “knowingly or intentionally” fails to comply with the statutory provision commits a Level 6 Felony. [48] Each day a violation of the duty statute continues is considered a separate offense. [49] In Indiana, a Class B Misdemeanor carries a penalty of imprisonment for a fixed term of not more than 180 days and a fine of not more than $1000, [50] and a Level 6 Felony carries a penalty of imprisonment for a fixed term between six months and three years, and a fine of not more than $10,000. [51] Neither the intent to transmit nor the actual transmission of HIV is required to be prosecuted under this statute. [52]
The “duty to warn” statutes make sense on their face, but no evidence exists to suggest these statutes fulfill their intent. Criminal consequences for a failure to disclose are intended by lawmakers to increase testing, encourage those who are positive to disclose, and thus decrease the number HIV infected persons. However, evidence and logic suggest the opposite is true. [53] People at risk are afraid to know their status in fear of being prosecuted.
Because public health is a significant state interest, one would think that state legislators would pass laws based on science and logic, not on fear of what or whom they do not understand. HIV is not easily transmitted, yet nearly seventy percent of states criminally target conduct unlikely to result in harm and increase criminal penalties for simply having HIV. [54] The first step in solving a problem is acknowledging there is one. States, including Indiana, must look beyond their own fear to see the “viral underclass” they have statutorily created. Having HIV or any disease should not be a crime.
[1] Sean Strub, Prosecuting HIV: Take the Test – And Risk Arrest?, Positively Aware (May/June 2012), http://www.positivelyaware.com/archives/2012/12_03/prosecutingHIV.shtml [https://perma.cc/3ZK7-RTYF].
[2] Sean Strub, Body Counts: A Memoir of Activism, Sex, and Survival 393 (2014).
[3] Id.
[4] H.R. Res. 1586, 114th Cong. (2015) (Introduced in Congress on March 24, 2015, this bill seeks to modernize laws and eliminate discrimination with respect to people living with HIV/AIDS).
[5] Infectious Diseases Society of America (IDSA) and HIV Medicine Association Position on the Criminalization of HIV, Sexually Transmitted Infections and Other Communicable Diseases, HIV Med. Ass’n (Mar. 2015), http://www.hivma.org/uploadedFiles/HIVMA/Policy_and_Advocacy/HIVMA-IDSA-Communicable%20Disease%20Criminalization%20Statement%20Final.pdf [https://perma.cc/G7AQ-WAN4].
[6] Id.
[7] Glob. Network of People Living With HIV, The Global Criminalisation Scan Report 2010 12 (2010), available at http://www.gnpplus.net/assets/wbb_file_updown/2045/Global%20Criminalisation%20Scan%20Report.pdf [https://perma.cc/X4CM-A44R] (reporting more than 300 people have been convicted under these laws in the United States and more than sixty in Canada).
[8] The Ctr. for HIV Law & Policy, Ending and Defending Against HIV Criminalization: State and Federal Laws and Prosecutions (May 2015), available at http://hivlawandpolicy.org/resources/ending-and-defending-against-hiv-criminalization-state-and-federal-laws-and-prosecutions [https://perma.cc/3E24-YVGZ].
[9] Id.; see also German Lopez, An HIV-Positive Man in Texas is Serving 35 Years in Prison for Spitting on a Cop, Vox (Feb. 19, 2015, 4:10 PM), http://www.vox.com/2015/2/19/8071687/hiv-criminalization [https://perma.cc/PP5Q-HLY5].
[10] The Ctr. for HIV Law & Policy, supra note 8; see also Diana Anderson-Minshall, Amazing HIV+ Gay Men: Nick Rhoades, Plus (Sep. 11, 2014 4:00 AM), http://www.hivplusmag.com/people/2014/09/11/amazing-hiv-gay-men-nick-rhoades [https://perma.cc/8NJX-L7EX].
[11] Id.
[12] The Ctr. for HIV Law & Policy, Ending & Defending Against HIV Criminalization: A Manual for Advocates 9 (2015), available at http://hivlawandpolicy.org/sites/www.hivlawandpolicy.org/files/HIV%20Crim%20Manual%20%28updated%205.4.15%29.pdf [https://perma.cc/S5D2-RHNU].
[13] See generally The Ctr. for HIV Law & Policy, Why Are We Putting People in Jail for Having HIV? (Nov. 2015), http://www.hivlawandpolicy.org/resources/why-are-we-putting-people-jail-having-hiv-a-grassroots-guide-hiv-criminalization-facts [https://perma.cc/DTF8-V7J9].
[14] Id.
[15] Id.
[16] Id.
[17] Pub. L. No. 101-381, 104 Stat. 576 (1990) (Congress reauthorized this act in 1996, 2000, 2006, 2009, and 2013).
[18] Who Was Ryan White?, Dep’t. Health & Hum. Servs., http://hab.hrsa.gov/abouthab/ryanwhite.html [https://perma.cc/7P2W-VKE5] (last visited Mar. 4, 2016).
[19] Ryan White CARE Act Celebrates 25th Anniversary, Dep’t. Health & Hum. Servs. (Aug. 18, 2015), http://www.hhs.gov/about/news/2015/08/18/ryan-white-care-act-celebrates-25th-anniversary.html [https://perma.cc/HQD4-4EQD].
[20] Id.
[21] Ryan White Comprehensive AIDS Resources Emergency Act of 1990 § 2647.
[22] Id.
[23] See Mich. Comp. Laws 333.5210 (2015).
[24] The Ctr. for HIV Law & Policy, supra note 12, at 292.
[25] Strub, supra note 2, at 393.
[26] HPV and Cancer, Ctrs. for Disease Control & Prevention, http://www.cdc.gov/cancer/hpv/statistics/cases.htm [https://perma.cc/TQY8-YQRM] (last updated June 23, 2014).
[27] Which Cancers Are Caused by HPV, Nat’l Cancer Inst., http://www.cancer.gov/about-cancer/causes-prevention/risk/infectious-agents/hpv-fact-sheet#q2 [https://perma.cc/M7K8-N7PT] (last reviewed Feb. 19, 2015).
[28] Cervical Cancer Statistics, Ctrs. for Disease Control & Prevention, http://www.cdc.gov/cancer/cervical/statistics/#2 [https://perma.cc/HV3Y-DNMZ] (last visited Dec. 9, 2015).
[29] HIV Among Women, Ctrs. for Disease Control & Prevention, http://www.cdc.gov/hiv/group/gender/women/ [https://perma.cc/9ED7-5ZJ6] (last reviewed Nov. 9, 2015).
[30] Id.
[31] Strub, supra note 2, at 393.
[32] Id.
[33] Ind. Code § 16-41-14-17 (2015).
[34] Id. § 35-42-2-1(b), (e), (g).
[35] Id. § 35-45-16-2(a)-(f).
[36] Id. § 35-42-2-1(b), (e), (g); id. 35-45-16-2(a)-(f).
[37] Ind. Code § 35-42-2-1(g).
[38] Id. § 35-42-2-1(d)(2).
[39] HIV and Its Transmission, Ctrs. for Disease Control & Prevention (July 1999), http://hivlawandpolicy.org/sites/www.hivlawandpolicy.org/files/CDC%2C%20HIV%20and%20its%20transmission.pdf [https://perma.cc/T2PQ-LPXC].
[40] Id.
[41] Id.
[42] Id.
[43] Ind. Code § 16-41-7-1.
[44] Id.
[45] Id.
[46] Id.
[47] Id. § 16-41-7-5.
[48] Id. § 35-45-21-3.
[49] Id.
[50] Id. § 35-50-3-3.
[51] Id. § 35-50-2-7(b).
[52] Id. § 16-41-7-1.
[53] HIV Medical Ass’n, supra note 5.
[54] The CTR. for HIV Law & Policy, supra note 12, at 292.
You can select your preferred language from the 'Select Language' menu at the top of the page.