Three years before the first federally funded community health centers in the US opened their doors to patients of all backgrounds, a 1962 law authorized the creation of new clinics to treat domestic migrant and seasonal agriculture workers.
The Migrant Health Act reflected a recognition that a community’s health depends on all who are a part of it, said historian Beatrix Hoffman, PhD, who studies immigration and health policy at Northern Illinois University. “The more people who have access to care, the better,” she added.
Migrant health centers served as a precursor to community health centers, which treat patients no matter their ability to pay. Today, community health centers across the nation are a major source of primary care for another migrant population: undocumented immigrants. But this could change with new restrictions from the US Department of Health and Human Services (HHS).
On July 10, HHS announced that undocumented migrants will no longer have access to any of the department’s taxpayer-funded services classified as federal public benefits. In addition to community clinics supported by the Health Center Program, this action affects services such as Head Start, certain substance use and behavioral health programs, and the Projects for Assistance in Transition from Homelessness grant program.
The new guidelines were enacted to “strengthen the integrity and consistency of benefit eligibility,” an HHS spokesperson said in a statement to JAMA Medical News. Public health experts, however, warn the change could undermine care through these programs for all patients.
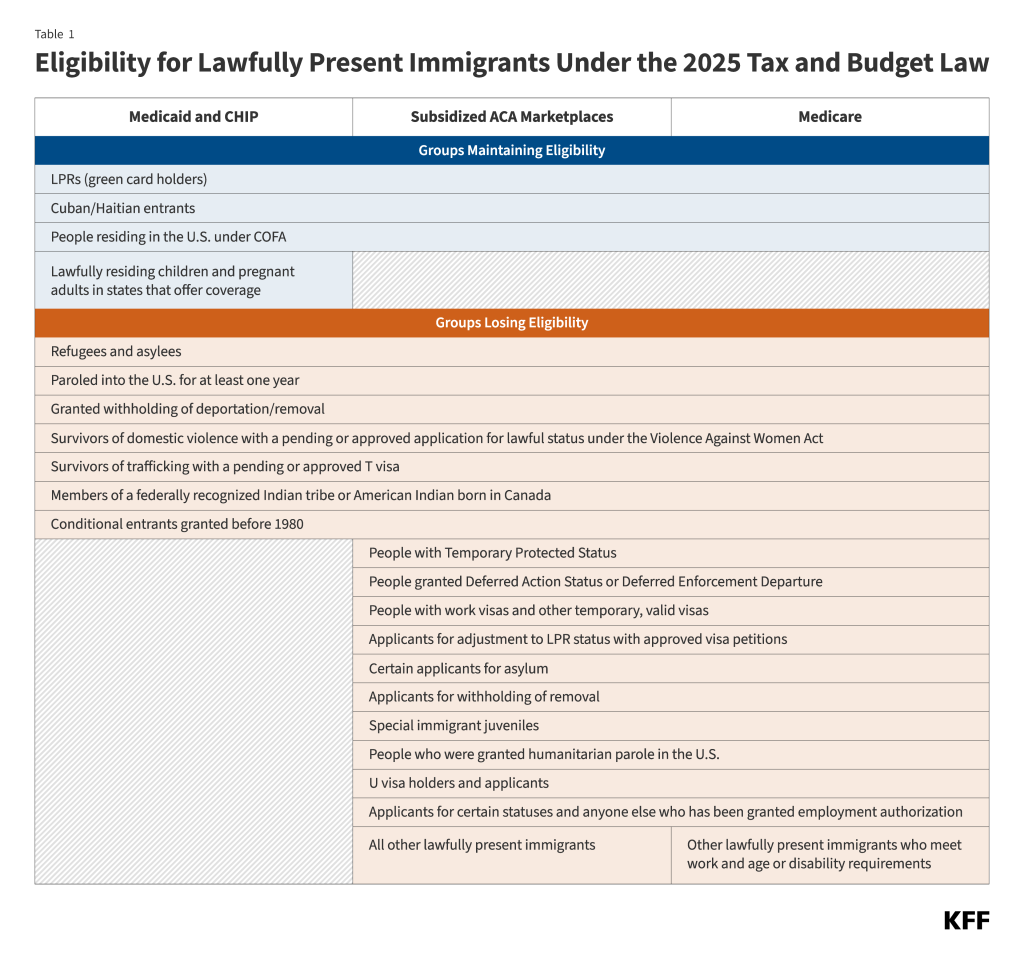
The new policy reverses a prior interpretation of the Personal Responsibility and Work Opportunity Reconciliation Act of 1996 (PRWORA), which allowed undocumented immigrants to access certain federal programs.
The change reflects the “taxpayer friendly” posture of President Donald Trump’s administration, said Ge Bai, PhD, CPA, an accounting professor at Johns Hopkins University and unpaid advisor to the Paragon Health Institute, a think tank founded by former Trump health care advisor Brian Blase. “The administration is facing the increasing deficit and worsening national debt, so they have to find all the ways they can to reduce government spending,” she said.
Undocumented immigrants pay sales tax on their purchases, and many pay income and property tax. Bai noted that these contributions do not make up a significant portion of the tax base. However, federal tax payments from undocumented immigrants totaled $59 billion in 2022, according to a report from the Institute on Taxation and Economic Policy.
The HHS has also stated that these services incentivize illegal immigration. Bai said that would-be migrants consider social programs when debating the risks and benefits of entering the country without authorization. She cited the influx of undocumented immigrants in 2021 through 2023, noting the expansion of the social safety net in response to the COVID-19 pandemic helped spark the migration surge.
Not everyone agrees. Although Hoffman allows that some undocumented immigrants may enter the country seeking specialized treatment, she countered that these cases are extremely rare. “Historically, undocumented people are afraid to access health care because they don’t want to be detected,” she said.
“People don’t migrate to the US to use health services or any other type of public benefit,” said Arturo Vargas Bustamante, PhD, MPP, a public health professor at the University of California, Los Angeles. “People migrate to the US because they have the economic incentive to get jobs.”
As undocumented immigrants tend to use fewer health services than US-born citizens and are ineligible for many federal programs including Medicare, Bustamante argued that their tax contributions subsidize health services for US citizens. A 2022 analysis in JAMA Network Openconcluded that tax contributions and premiums from undocumented immigrants exceeded expenditures by more than $4000 per person.
Bustamante said the benefits of offering services such as vaccinations and prenatal consultations to undocumented immigrants outweigh costs to taxpayers. He doubts the new guidelines will curb health care spending, in part because it could increase reliance on emergency care. Emergency departments remain open to undocumented immigrants because of the Emergency Medical Treatment and Labor Act, which prevents hospitals that receive Medicare dollars, as the overwhelming majority do, from refusing to treat patients in emergency conditions. There, care may be covered by emergency Medicaid that is available regardless of immigration status with qualified expenses varying by state.
Without primary care services through community health centers, Bustamante and others predict that undocumented immigrants will forgo treatment for as long as possible until they require emergency care.
“They won’t go to get medication. They won’t go to get regular checkups. They won’t go to get preventive care,” said Annie Ro, PhD, associate professor at the University of California Irvine Joe C. Wen School of Population and Public Health.
Losing access to primary care leaves people with fewer options to manage chronic conditions, which can lead to new health problems like infectious disease, said Nicole Swartwood, MSPH, who studies public health at Harvard University.
For example, unmanaged diabetes might increase the odds that a latent tuberculosis infection will become active and contagious—and individuals born in many countries outside the US are already at greater risk of tuberculosis.
Homelessness and intravenous drug use are also linked to tuberculosis, Swartwood added. The new restrictions would block undocumented immigrants from HHS services related to those concerns as well.
Meanwhile, community health centers play a role in infectious disease surveillance, including screening for asymptomatic latent tuberculosis. If undocumented patients are barred from these clinics, their condition may not be identified and they may transmit tuberculosis to others. “Nondocumented migrants are not living in isolation,” said Swartwood, adding that they are part of their communities and interact with others.
Impaired infectious disease monitoring is just one way the HHS policy may affect more than just undocumented immigrants. Multiple experts said they worry the new rules will sow fear that deters migrants from accessing care even when they qualify for it.
Ro pointed out that many undocumented immigrants have children who are US citizens by birth. “These kids are not targeted by these restrictions, but because their parents are concerned, we’ll probably see a chilling effect within families,” she said.
Determining eligibility could itself pose a challenge for clinics. “Providers are legally bound to provide care when it’s needed, but they’re put in this position where they have to verify somebody’s immigration status,” Ro continued. “That’s not really their job.”
HHS has not yet released program-specific guidance, but Ro fears that calling on understaffed clinics to enforce these restrictions will divert time and resources away from patient care.
“Everyone is going to be affected, not only immigrants themselves, but also migrant families, mixed-status families, and US-born citizens who are going to encounter more expensive health services, longer waitlists, and less provider availability,” Bustamante said.
The HHS rules are not the only rollback of services for undocumented immigrants this year. California, Illinois, and Minnesota have each scaled down or cut eligibility for state Medicaid coverage previously offered to immigrants of any status.
In April, the Idaho state legislature passed HB 135, which excluded undocumented immigrants from services such as food pantries and prenatal care. Controversially, the bill originally required proof of legal status from patients receiving medication at programs funded through Part B of the federal Ryan White HIV/AIDS Program.
“HIV is very treatable, and we have great medications for it,” said Abby Davids, MD, MPH, who treats patients with HIV at a federally qualified community health center in Boise. “But if you lose access to your antiretrovirals, then HIV is universally fatal.”
Davids added that without medication, people living with HIV could transmit the virus to others: “From an individual patient standpoint and from a community standpoint, it’s a really horrific situation.”
The portion of HB 135 restricting HIV treatment was blocked by a federal judge in late June following a lawsuit by the American Civil Liberties Union on behalf of Davids and 5 unnamed patients. The next month, a federal judge granted a preliminary injunction preventing immigration status–based restriction to Ryan White Part B programs until all litigation is settled.
HHS has not responded to requests from JAMA Medical News for comment about how eligibility for Ryan White–funded programs may change because of the new federal guidelines.
Undocumented immigrants can still receive emergency Medicaid in all 50 states, although the Centers for Medicare & Medicaid Services has agreed to share information about Medicaid enrollment with Immigrations and Customs Enforcement, the Associated Press reported in July.
“This administration has been so aggressive in targeting any kind of benefit that would remotely touch the undocumented immigrant population,” Ro said.
Published Online: August 8, 2025. doi:10.1001/jama.2025.12999
Conflict of Interest Disclosures: None reported.