Can this HIV prevention strategy overcome mistrust and fear among marginalized communities?
In Texas, health officials recently used a new surveillance technology to identify a large HIV outbreak among gay and bisexual Latino men. In Massachusetts, officials used the same strategy to respond to an outbreak among injection drug users. And in California, researchers used the method to identify a transmission cluster among transgender women.
Led by initial proof-of-principle research at the Centers for Disease Control and Prevention (CDC), an HIV prevention strategy known as molecular surveillance is quickly expanding across the country. Since December 2015, according to an email from a CDC source who commented on background, the technique, based on sequencing and comparing individuals’ viral genetic blueprints, has identified more than 240 recent and rapidly growing HIV transmission clusters, the vast majority of which had not previously been recognized. Comparing these sequences allows researchers to determine whether individuals’ HIV is closely related, which offers clues about who transmitted the virus to whom.
Traditional public health methods—now being used to trace the spread of COVID-19, the disease caused by the new SARS-CoV-2 coronavirus—largely rely on asking people about their contacts and getting in touch with them by phone or in person. The CDC source said molecular data analysis allows for more rapid and comprehensive cluster and outbreak detection and response. As such, molecular surveillance is seen by the agency as a key part of effective HIV prevention and a means to help hard-hit communities and the nation end the HIV epidemic.
Those idealized goals, however, are clashing with a far messier reality in which decades of mistrust and fear among marginalized communities, heightened in the current political climate, are coming to a head. The tech-aided HIV surveillance strategy, six activists told POZ, could open up new avenues for private data to be breached, exploited, subpoenaed or otherwise released through many of the HIV criminalization laws and statutes still on the books in 34 states.
Activists say the CDC-led molecular surveillance effort was launched with little or no consultation or buy-in from the communities most likely to be impacted. Several meetings ensued, including one convened in 2018 by the O’Neill Institute for National & Global Health Law at Georgetown Law School in Washington, DC, that allowed critics to air some of their concerns. Despite a subsequent round of CDC guidelines on how best to safeguard patient data, however, the controversy has only grown over the potential misuse and unintended consequences of the surveillance scheme.
Patients can’t opt out of providing their viral sequence data for the molecular tracking, critics point out. Nor does the strategy adequately consider the state-by-state patchwork of protections and penalties or the growing health implications of an erosion of immigrant, minority and LGBTQ rights, they say.
Sean Strub, POZ’s founder and the executive director of the nonprofit Sero Project, which focuses on reforming HIV criminalization laws, says he fears the CDC-led strategy will diminish trust and cooperation with public health agencies and drive more vulnerable people further from the health care system out of fear of surveillance. “I think the risk of unintended consequences is very great,” he says.
Strub and other activists see molecular surveillance as part of a broader trend in the “securitization of disease,” which is increasingly blurring the lines between the public health and criminal justice systems.
“We are potentially threatening people’s freedom just to get cleaner data, and I think it’s a clear ethical concern,” says Devin Hursey, a member of the Missouri HIV Justice Coalition and a board member of Blaq Out, a nonprofit advocacy group for Black queer and transgender people in the Kansas City region. “We can’t just look the other way or say we’re doing our best effort when we’re not really addressing that HIV criminalization still exists.”
The CDC source told POZ that the agency understands and has addressed many of the questions and concerns raised by community advocates. The CDC has strong data protections and security measures in place, the source said, and has worked for many years to provide guidance to states on reviewing and revising criminalization laws and ensuring data are well protected.
But Naina Khanna, executive director of Positive Women’s Network–USA, says the CDC hasn’t responded to specific questions about its data-sharing practices with other federal agencies, like the Department of Homeland Security and Immigration and Customs Enforcement (ICE). Khanna points out that the communities most impacted by HIV are also disproportionately affected by surveillance, policing and criminalization. “That’s extremely concerning when we think about how policing intersects with being a Black gay man or being a Latino gay man,” she says. In response, the CDC source told POZ that all HIV surveillance data are reported to the agency without names or any personal identifiers and are encrypted and protected by an Assurance of Confidentiality under Section 308(d) of the federal Public Health Service Act.
A New Surveillance Tool
When someone tests positive for HIV in the United States, a blood draw allows labs to sequence part of the viral genome, or its genetic blueprint, and use that to determine whether the virus contains mutations that might lead to drug resistance. This information can help doctors tailor the best HIV treatment regimen for each individual. But once the genetic sequencing is complete, health departments can access that data for molecular HIV surveillance. Specifically, they compare viral RNA sequences from multiple individuals to identify clusters of transmission. This is possible because HIV mutates over time; as a result, people with similar genetic sequences are more likely to have been infected around the same time as part of the same person-to-person chain of viral transmission.
Randy Mayer, MS, MPH, chief of the Bureau of HIV, STD and Hepatitis at the Iowa Department of Public Health, says the HIV resistance tests sent in by doctors around the state essentially provide his department with free surveillance data. “It’s something that we can use to try to improve our response that doesn’t really cost us anything,” Mayer says. “So from that point of view, it is cost effective.”
If a state-run computer program finds two or more individuals who share closely related viral sequences, it suggests that HIV might have passed between them or through a close intermediary. Spotting such clusters of transmission could help public health officials identify HIV-positive individuals and their close sexual or needle-sharing partners.
The surveillance approach has multiple potential benefits, researchers say. “This is just one more strategy in the toolbox of surveillance tools used to guide public practice,” says Nanette Benbow, MAS, research assistant professor of psychiatry and behavioral sciences at Northwestern University Feinberg School of Medicine in Chicago. HIV transmission clusters identified through this method, she says, may represent only the “tip of the iceberg” of at-risk individuals, since the genetic information is available only for HIV-positive people who’ve been to a doctor and received drug resistance testing. Through contact tracing, though, public health officials can find other people associated with the cluster, contact them and offer them a range of care or prevention services, like pre-exposure prophylaxis (PrEP), if they’re not already receiving them.
Benbow says evidence suggests that the rate of HIV transmission within such clusters is much higher than that of transmissions overall, bolstering the case that public health agencies should focus on these clusters as significant sources of active viral transmission.
Some public health experts say the growth of surveillance is inevitable. “You’re not going to stop technology. All you can do is try to get it implemented in an ethical manner,” says Eve Mokotoff, MPH, managing director of HIV Counts, a consulting business based in Ann Arbor, Michigan, that assists with HIV surveillance.
Andrew Spieldenner, PhD, vice chair of the U.S. People Living with HIV Caucus and an assistant professor of communications at California State University San Marcos, rejects that argument. “Just because technology exists doesn’t mean we have to use it,” Spieldenner says. “We have to balance it with the harms it does to individuals.”
Newer technology that could extend molecular HIV surveillance is giving activists more pause. One method, called ultra-deep whole-genome next-generation sequencing, isn’t yet part of the CDC strategy. But emerging study data suggest that it could predict the directionality of linked HIV transmissions, potentially adding new evidence to suggest who infected whom. Researchers at Johns Hopkins University School of Medicine, in fact, recently described how they correctly predicted HIV transmission from an index case to a sexual partner in more than 90% of 105 sample pairs. The direction couldn’t be established in the remaining cases, but the method didn’t incorrectly predict any transmissions.
Other research the CDC is pursuing may help estimate the recency of an infection, meaning whether one person acquired HIV more recently than another. Together, the data could enable additional predictions about when and how HIV infections occurred within transmission clusters. Benbow says the data on their own don’t prove direct transmission, since another individual could have been an intermediary in the chain, but Khanna points out that judges and juries wouldn’t necessarily take these scientific caveats into account. “We see a lot of potential for opening the door to criminalization,” she says.
Despite privacy assurances, Strub maintains that data collected for one purpose is being unethically used for another without patient consent. “It’s not being used evenly across the society. Molecular surveillance focuses on the communities that are already highly marginalized, communities where there is the greatest risk of serious, harmful consequences,” he says. “People of privilege don’t see this.”
In a 2019 letter in the journal Lancet, researchers at the University of California, San Diego responded to criticism of their molecular surveillance study of an HIV transmission cluster involving transgender women by questioning whether informed consent is “imperative” for such analyses. “Surveillance for numerous infectious agents, including HIV, is done ethically and without consent. The public good of HIV surveillance justifies this approach,” they wrote. “Requiring consent for surveillance reporting would preclude a robust understanding of disease distribution and spread and the ensuing benefit to the health of individuals and communities.”
Alexander McClelland, PhD, a postdoctoral researcher in the Department of Criminology at the University of Ottawa, says such arguments reflect the logic that people living with HIV are an “object of risk” to be managed by public health. “We’re not considered to be people who have autonomy or rights to privacy or security of our own lives and our own bodies and our own data,” he says.
Many defenses of molecular surveillance, McClelland adds, also overlook other implications beyond the “broader public good” of repurposing patient data for public health surveillance. Among them, he says, are the criminalization, uncertainty and fear of people who are living with HIV and subject to continual privacy breaches. “People love to say, ‘We’re looking at molecules not people.’ But those molecules are connected to people, and those people are in the social world,” McClelland says, “and you can’t evacuate a virus from the social context that it’s in.”
A Climate of Fear
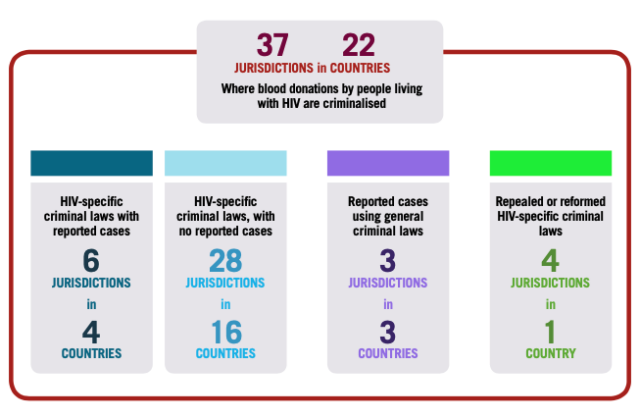
According to the Center for HIV Law & Policy in New York City, 34 states have enacted some form of HIV criminalization law or sentencing enhancement for other crimes allegedly committed by a person living with HIV. Although the language varies, 21 states have laws under which HIV-positive people who are aware of their status but don’t disclose it to sexual partners can be prosecuted (additional states have prosecuted nondisclosure under different laws); 12 states require the same disclosure among people who share needles. Some laws cover alleged HIV exposure while others cover actual transmission. Between 2009 and 2019, 24 states also prosecuted people living with HIV under other criminal statutes.
The interpretations and enforcement of laws can vary widely as well. In an April 2020 report, the Williams Institute at the UCLA School of Law documented 209 arrests and 107 convictions under Missouri’s HIV criminalization laws between 1990 and 2009. The report noted that the crimes appeared to be disproportionately enforced in St. Louis and adjacent St. Louis County. Although Black men account for 5.5% of Missouri’s population and 35% of people living with HIV, the report found, they accounted for more than half of HIV crime arrests and convictions over the 20-year period.
“We’re oftentimes targeted by not just HIV laws but by a lot of other different laws. We’re more likely to experience surveillance by law enforcement,” Hursey says of Black men. Layering on the element of molecular surveillance, he adds, only compounds the fear and lack of trust in public health and discourages the honest answers and cooperation necessary for HIV peer educators like him to do their jobs effectively. That mistrust is heightened by the legal requirement that Missouri’s health department must turn over all surveillance data to prosecutors pursuing an HIV criminalization case, he says.
“We have an epidemic of criminalization of people living with HIV, and you can only be prosecuted or convicted if you know your HIV status,” Khanna says. If people already feel marginalized and stigmatized, she and Hursey say, the added threat of criminalization based on knowing their HIV status can deter them from ever seeking out testing or care—the very opposite of stated public health goals.
Marco Castro-Bojorquez, cochair of the HIV Racial Justice Now project, says molecular HIV surveillance could likewise put undocumented immigrants at risk, especially since their existence in the United States is already criminalized. “It’s problematic, and it breaks my heart because a lot of people that could be very affected are those that are so fearful of the government and don’t really know that it’s happening,” he says.
Across the border from Missouri, Mayer says public health data are “well protected” in Iowa. They weren’t always, but in 2014, Iowa reformed its HIV criminalization law. The updated statute, Mayer says, requires proof that an HIV-positive person was negligent in exposing a partner to the virus and prohibits molecular surveillance data gathered by the state health department from being used to prosecute anyone. “I had some upset prosecutors who have tried to come to me, with subpoenas, to get information, which we don’t allow,” he says. Prosecutors can gather the data from other sources, but the health department has largely cut its tether to law enforcement.
Even so, prosecutors have found other mechanisms to gather data and enforce Iowa’s HIV criminalization law. In May, a 33-year-old Black man was sentenced to 26 years for “knowingly” exposing three women and a minor to HIV and transmitting the virus to three of them.
Activists say public health agencies also cannot divorce their molecular surveillance plans, however well intentioned, from the current rollback of LGBTQ, immigrant and minority rights. Castro-Bojorquez says the Trump administration’s anti-immigrant rhetoric and policies have not only eroded the Latino community’s trust in public officials but also worsened health outcomes. “Those attacks,” he says, “and the promotion of hatred, rolling back the few rights that we had and we fought so hard for, they have an impact, and people die.”
Numerous undocumented immigrants held in crowded detention centers have contracted COVID-19, and some deported immigrants have brought the coronavirus back to Guatemala, Mexico and other countries. Fear of HIV criminalization or deportation, Castro-Bojorquez says, has led other immigrants to avoid or delay “official” activities, including HIV testing and treatment. “Late diagnosis is a major issue in our communities,” he says, adding that it’s a big contributor to higher mortality rates among Latino men.
***
Finding Common Ground
Amid the ongoing controversy, HIV activists and public health officials may be finding common ground on the need for more community engagement and on the importance of decoupling public health and law enforcement. In a 2019 commentary in the American Journal of Public Health, Benbow joined other AIDS researchers, bioethicists and a representative of the National Alliance of State and Territorial AIDS Directors (NASTAD) in explaining how multiple aspects of existing HIV criminalization laws could confound public health goals around molecular surveillance.
Benbow and her coauthors cautioned that using identified surveillance data against the interest of patients, especially without informing them, “could jeopardize community confidence in public health agencies.” The authors also noted the CDC’s requirement that funded health departments create plans to address gaps in data protection and consider eliminating or modifying potentially counterproductive laws. “In light of the considerations we have addressed, health department leaders should consider supporting statutes that expressly limit, or even prohibit entirely, release of surveillance data for law enforcement purposes,” they wrote.
Mokotoff cautions that a health department can’t always change its state law. “But the health department can work with the community to help them understand what needs to be done and what kind of wording might be helpful,” she says. “We have to stop allowing surveillance data to be used for prosecution of people who are sick or infected.” Protecting that data from being used in law enforcement, she adds, “would change the entire discussion” with stakeholders in the HIV-positive community.
The CDC itself has avoided criticizing specific state laws, though the agency source told POZ that the CDC has worked with partners like NASTAD to review the range of legal protections, policies and procedures that can help protect HIV data. The source noted that in 2014, the Department of Justice recommended that states either reform their laws to eliminate HIV-specific criminal penalties or modernize their laws to reflect current scientific evidence. The source also pointed out that the Department of Health and Human Services 2019 initiative, “Ending the HIV Epidemic: A Plan for America,” encourages states to take similar steps to help reduce stigma.
Benbow conceded that addressing the intense mistrust of underserved individuals who may need HIV prevention or treatment services the most, including people who inject drugs and undocumented immigrants, remains a steep challenge. But identifying clusters, she says, could help health officials make the case for targeted services that benefit underserved people, like the legalization of needle exchange programs.
“A lot of what we do in public health infringes on privacy, and what we’re trying to do is balance a person’s individual freedoms and liberties and privacy with trying to improve public health and work for the common good,” Mayer says. “You really have to think very carefully about that because if you push that too far, then you’re likely to get a lot of public health interventions rolled back, and people don’t want to work with you. They don’t trust you.” And as the history of HIV shows, regaining lost trust can take decades.