A newly published report suggests a number of concrete ways that research into the impact of overly broad HIV criminalisation on public health can move the policy agenda forward, and help reform laws and create better policies for people living with HIV and most affected communities.
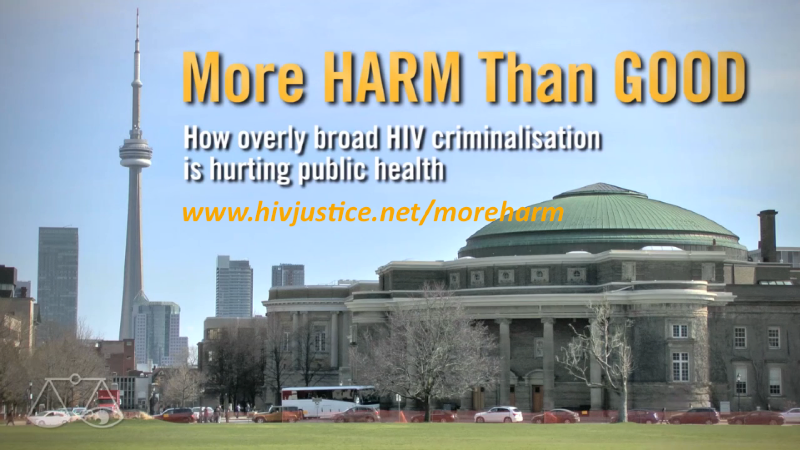
The report is the result of an international workshop on HIV Prevention and the Criminal Law held in Toronto, Canada on April 27th and 28th 2013 that also led to the creation of the HIV Justice Network’s video documentary, More Harm Than Good.
The workshop’s aim was to support, encourage and further develop emerging research on the public health implications of criminalising HIV non-disclosure, exposure and transmission. It was the first international meeting focused exclusively on sharing, critiquing and strengthening new empirical research on this topic.
The report explores three key themes that arose over the course of workshop discussions – (1) the relationship between research and advocacy; 2) the implications of HIV-related criminalisation for public health practice; and (3) the potential and limits of public health research for criminal law reform – and offers suggestions for new directions for future research on the public health implications of criminalizing HIV non-disclosure, exposure and transmission.
Workshop discussions emphasised that research on the public health implications of HIV-related criminalisation is able to do the following:
- Identify the impacts of HIV-related criminalisation on HIV prevention, care, treatment and support. Research into such impacts is especially important in light of new approaches that respond to the HIV epidemic by increasing the uptake of HIV testing and counselling, linking HIV-positive people to health and social services, initiating HIV antiretroviral therapy as early as possible, and retaining people living with HIV/AIDS in medical care.
- Elucidate the influence of criminalising HIV non-disclosure, exposure and transmission on the attitudes, opinions, beliefs and activities of people living with HIV/AIDS, people and communities at risk, service providers in public health and clinical settings and staff in ASOs and community-based organisations.
- Inform efforts to respond to the potential discriminatory enforcement of criminal laws by identifying the demographic patterns associated with HIV-related criminal prosecutions.
- Provide public health authorities with evidence required to become more engaged in the issue, to develop policy and programmes, and to comment publicly on an increasingly important facet of the HIV epidemic.
- Identify legal, ethical and practice issues faced by public health and clinical staff as a result of HIV criminalisation, and provide evidence to support legally and ethically sound policy and practice.
- Assess the efficacy and costs and benefits of different policy options to address HIV transmission.
- Inform decisions by legislators, criminal prosecutors and courts in a number of jurisdictions.
The meeting identified five main suggestions for moving the research field forward.
1. Explore novel analytical and methodological approaches
Given the complexity of HIV criminalisation, applied and theoretical research agendas should be structured broadly, inquire into a wide range of possible “implications” and account for the intersectionality of factors such as race, class, migration, colonisation and gender. New research would benefit from a deeper engagement with socio-legal studies and criminology.
Further suggestions:
- Ground research questions in a health and human rights or an intersectional/anti-oppression framework as alternatives to a public health implications framework.
- Critically engage with mainstream feminist analysis that supports HIV criminalisation.
- Use qualitative approaches, including narrative analysis, ethnographic methods and participatory action research to:
- Capture issues of importance to, and respond to the needs of, communities of people living with and at risk of HIV;
- Document and explore experiences of people who have been criminally charged and/or prosecuted as well as those who have brought forward police complaints;
- Explore HIV criminalisation as a complex, constructed and varied social phenomenon.
2. Conduct intervention research
Research on the public health implications of criminalising HIV non-disclosure would be enhanced by studies exploring the processes and outcomes of interventions that offer alternatives to criminalisation and/or that seek to prevent HIV transmission.
Further suggestions:
- Conduct research on and explore the implications of using restorative justice approaches for criminal offences related to HIV non-disclosure, exposure and transmission.
- Evaluate the impact of new or existing case management strategies that focus on sexual activities that risk incarceration and HIV transmission:
- Explore collaborations with HIV/AIDS Service Organisations (ASOs) and other community-based organisations as sites for intervention research. ASOs offer a less coercive and more supportive environment to address challenges of concern to the public health and the criminal justice systems;
- Conduct ethnographic research on the “Calgary Model.” (See ‘A framework to consider for the non-disclosure of HIV/AIDS – the Calgary Health Region model’ halfway down this page) The Calgary Model is a policy-informed public health case management model that has been endorsed by policy makers in Canada, yet has not been empirically studied.
3. Conduct research on factors that underpin and drive HIV criminal prosecutions
Research on the criminalisation of HIV non-disclosure, exposure and transmission has yet to rigorously explore the various factors that encourage criminal prosecutions. There has been very little research involving people who initiate criminal complaints, their motivations
for doing so, their relationships with people living with HIV/AIDS and their experience of the criminal justice system. Relatedly, we know very little about police and prosecutors, their understandings of laws related to HIV non-disclosure, exposure and transmission, their knowledge of HIV and HIV transmission, and their attitudes towards people living with HIV/AIDS. There is a strong need for research that explores the underlying social, structural, behavioural and cultural factors that drive HIV-related criminalisation.
Further suggestions:
- Prioritize police, prosecutors and complainants in new research.
- Conduct research on the moral and other discourses that underpin criminalization and that inform the perspectives of the general population, those living with and at risk of HIV, legislators and policy makers and those who work in the criminal justice and public health systems.
Potential research foci include:
- norms of sexual practice in communities as contrasted with principles of “good behaviour” applied by courts;
- lessons from harm reduction and drug policy reformists who have had some success in working with police in opposing drug prohibition and the “war on drugs”;
- critical analysis of how the “good versus bad” person living with HIV/AIDS is discursively constructed in media and elsewhere;
- how issues of “personal responsibility” and “wrong” conduct get constructed, expressed and enacted, and to what end;
- redesigning existing quantitative surveys to more robustly inquire into the attitudes, opinions and beliefs of respondents;
- a moral mapping and deconstruction of pro-criminalisation arguments.
4. Continue to research the implications of criminalization for those who work in HIV prevention and in clinical and support services for people living with HIV/AIDS
Additional research on how criminalisation affects the work of various practitioners engaged in HIV prevention and the treatment, care and support of people living with HIV/AIDS can further our understanding of the broad implications of criminalizing processes. Comparative studies across national jurisdictions would yield important results.
Further suggestions:
- Build on existing studies by incorporating mixed methodologies into research designs:
- Investigate innovative and more rigorous approaches to sampling than has been the case in existing studies.
- Explore how changes in front-line practice related to criminalisation may be connected with broader policy and program changes.
- Investigate the discursive and other bases of public health response (e.g. explore the origins and impact of “unwilling and unable” terminology in Canadian public health policy).
5. Conduct media research
The mass media are an important source of public information about the criminalisation of HIV non-disclosure, exposure and transmission. While we have many accounts of how the media coverage of HIV criminal cases contributes to HIV-related stigma, we have little published research that draws on rigorous sampling methods to explore this question.
Further suggestions:
- Conduct research to understand the impact of media coverage on communities and people living with and affected by HIV, the general public and legal and policy decision makers.
- Inquire into the association between media coverage and stigma especially in relation to African, Caribbean and Black communities.
- Systematically analyze the narrative and rhetorical conventions used by mainstream media when reporting on and editorialising about HIV criminal cases.
- Investigate the use of media by police as an investigative tool.
This article is only a summary of the highlights of the report, and the entire meeting report is well worth reading.
The Criminalization of HIV Transmission and Exposure Working Group from Yale University’s Center for Interdisciplinary Research on AIDS (CIRA) have also published a research agenda focused primarily on the the research needs of advocates in the United States. This was based on a meeting held in November 2011 and authored by some of the same participants that attended the Toronto workshop, including Carol L. Galletly, Zita Lazzarini and Eric Mykhalovskiy.
This meeting concluded that the research agenda should include studies of:
(1) the impact of US HIV exposure laws on public health systems and practices;(2) enforcement of these laws, including arrests, prosecutions, convictions, and sentencing; (3) alternatives to HIV exposure laws; and (4) direct and opportunity costs of enforcement.
You can read the full research agenda, originally published in the American Journal of Public Health in August 2013, below.
Criminalization of HIV Transmission and Exposure – Research and Policy Agenda (August 2013)