Speech delivered on the final morning plenary session of the 16th AIDSImpact Conference, Casablanca, 28th May 2025
Good morning.
I am deeply honoured to stand here with you today in Casablanca – a city whose name evokes stories of resistance and solidarity – to share our own story of resistance and solidarity: the global movement to end HIV criminalisation.
It’s especially meaningful to be back at AIDSImpact. Because, you see, this is where it all began for me. Eighteen years ago, in Marseille, I stood on a stage like this one, trembling slightly, as I spoke publicly for the very first time about HIV criminalisation.
I had no idea that moment would change the course of my life – or that it would help spark a movement that continues to grow today.
Later that same year, NAM – where I worked as an HIV treatment journalist – published my first book on the subject aimed at explaining HIV science and social science to the criminal legal system, and I started a blog – Criminal HIV Transmission – as a way of documenting the mounting number of unjust prosecutions and problematic new laws taking place across the world.
What started as a mostly solitary – and primarily UK-focused – effort quickly became a shared and surprisingly international one.
By AIDS 2008 in Mexico City, I began to understand that my blog was becoming a de facto global network, and many of the cases it documented were cited by South African Justice Edwin Cameron when, during his now-legendary plenary, he called for a global movement to end HIV criminalisation.
That same year UNAIDS and UNDP released guidance opposing overly broad criminal laws, and it was clear that something was shifting.
Two years later, at AIDS 2010 in Vienna we – that is NAM, GNP+, and the Canadian HIV/AIDS Legal Network – convened the first-ever pre-conference on HIV criminalisation. It brought together scientists, advocates, lawyers, and most importantly, people living with HIV. I had planned to start the HIV Justice Network then, but a consultancy job at UNAIDS, providing scientific and legal support for clear guidance to limit the overly broad use of the criminal law, kept me busy.
So it wasn’t until 2012, when we gathered in Oslo at a UNAIDS consultation on HIV and the criminal law, that the network finally came together. On the sidelines of the consultation, key representatives of civil society worked together to draft the Oslo Declaration on HIV Criminalisation – a ten-point call to action that was endorsed by more than 1700 individuals and organisations from 130 countries and, to my astonishment, also appeared as an appendix to the official UNAIDS guidance note that was published in 2013.
The Oslo Declaration became the founding document of the HIV Justice Network. From that point on, we were no longer reacting – we were organising.
By AIDS 2014 in Melbourne, with the support of several Australian and international HIV organisations, we held the Beyond Blame pre-conference, where our first major victory was announced: the repeal of the Australian state of Victoria’s HIV-specific criminal law. We knew then that change was possible.
In 2015, we joined forces with ARASA, the HIV Legal Network, GNP+, the Sero Project, and Positive Women’s Network–USA to form a powerful global consortium. With support from the Robert Carr Fund, we launched the HIV JUSTICE WORLDWIDE coalition in 2016, committing ourselves to collective action against the unjust criminalisation of people living with HIV.
Together, we developed a range of advocacy tools and resources, including the Expert Consensus Statement on the Science of HIV in the Context of Criminal Law, launched at AIDS 2018 in Amsterdam. The Consensus Statement translated complex science – about viral load, transmission routes, treatment effectiveness, and HIV forensics – into language that courts and lawmakers could understand.
Because the truth is: the law had not kept pace with science. Outdated laws continued to criminalise people living with HIV as though it were still the ‘90s. And behind each of these prosecutions was a human life: interrupted, humiliated, punished, often for simply living with a virus.
Today we know that people living with HIV on effective treatment cannot transmit the virus. U=U is not just a slogan – it’s a scientific fact. And that message has been useful in limiting unjust prosecutions, primarily in the global North.
But HIV criminalisation is a global phenomenon, and we cannot rely on science alone as an argument against HIV criminalisation, especially in places where access to treatment or viral load testing is limited or is being taken away; nor in this brave new world of integration, where treatment or prevention is only likely to be accessed by people who are not marginalised, stigmatised, or otherwise criminalised.
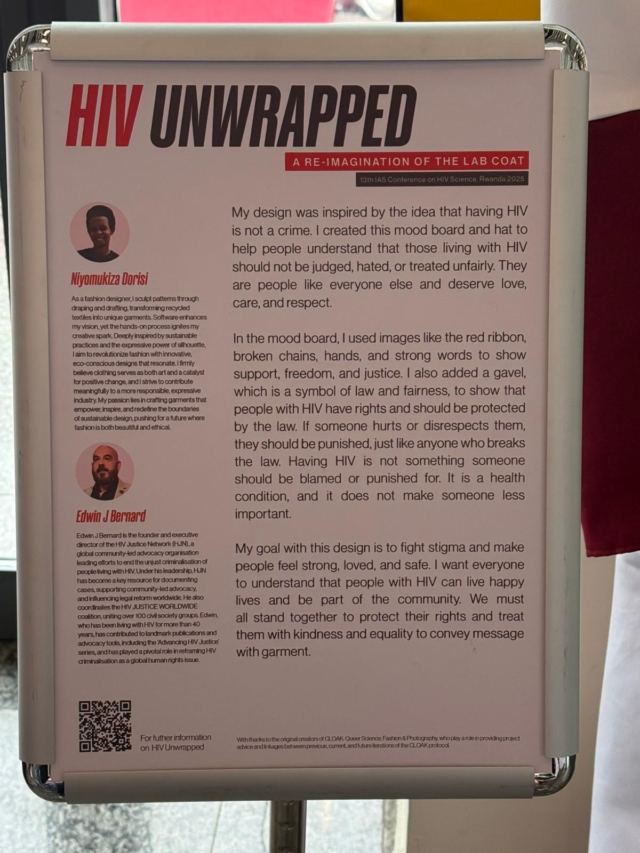
That’s why our key messaging must always be that making people living with HIV solely responsible – and criminally liable – for HIV prevention is simply wrong: it’s ineffective, counterproductive, and unjust. That’s where storytelling comes in – to shine a spotlight on the human cost. So over the years we made documentaries focusing on the impact of HIV criminalisation on people.
Documentaries like More Harm Than Good – which brought to life all the social science studies that overwhelmingly found mandating disclosure, criminalising non-disclosure, and sending people to prison for potentially exposing or allegedly passing on HIV did the opposite of what lawmakers intended.
And Mwayi’s Story, about a woman in Malawi unjustly prosecuted for briefly comfort-nursing another woman’s baby and the subsequent empowered movement of women living with HIV in Malawi who spoke truth to power and persuaded their Parliament not to pass an HIV-specific criminalisation law.
We wanted to show that these laws and prosecutions do nothing to protect public health – in fact, they undermine in, and they destroy lives in the process. They increase stigma, turning vulnerable people away from prevention, treatment and care services.
And we have never stopped centring the voices of those most harmed.
People like Rosemary Namubiru, a kind, elderly nurse in Uganda, who dedicated her life to caring for others. She was falsely accused of exposing a child to HIV while administering an injection – a claim later shown to be scientifically impossible. Yet she was arrested live on TV, vilified in the press, and imprisoned. Rosemary was a survivor, but she never recovered from what was done to her. When she passed away in 2022, she left behind not only grief and anger, but also a legacy – a reminder of why we do this work. To honour her. To fight for the dignity and rights of people like her. And to ensure that no one else is ever treated the way she was.
And here in Morocco – where people living with HIV and key populations still face stigma, criminalisation, and exclusion – we must also honour the rich legacy of resistance, solidarity, and resilience that continues to inspire advocates demanding justice, dignity, and change.
Throughout this movement, it has always been communities who’ve led the way: survivors who dared to speak their truths; advocates who pushed for reform; scientists who stood up for evidence-based policy; and networks like ours, who bring it all together.
I never imagined, back in 2007, that this would become my life’s work. But here I am, 18 years later, standing before you with immense pride in what we’ve achieved – and profound concern for what we’re up against. Because the truth is: we are facing an existential moment.
Globally, we’ve witnessed the rise of authoritarianism and the anti-rights movement, which along with the funding crisis is leading to a rollback of hard-won human rights, and the erosion of multilateral cooperation.
Some governments are already doubling down on criminalisation – of people and of NGOs – using stigma and fear to justify their repression. And I worry that punitive approaches to HIV prevention will become the new normal, including policing of the bodies and lives of people living with HIV that was considered acceptable in the ‘90s.
And people living with HIV – especially those who are Black, Brown, gay or queer, trans, migrants, sex workers, people who use drugs – will be the first to be caught in the crosshairs.
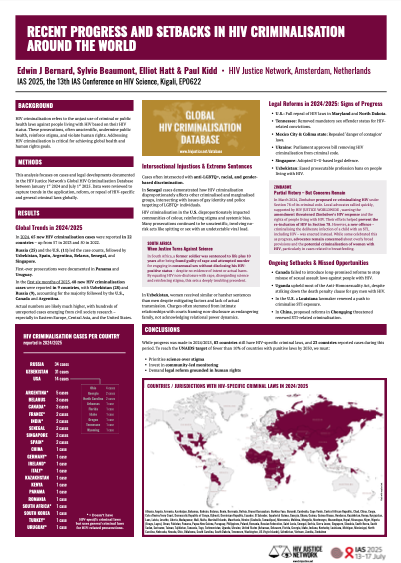
The HIV justice movement was born out of crisis, but it is sustained by hope. We know change is possible – because we’ve seen it, even under the most difficult conditions. In fact, over the past five years 25 jurisdictions in 11 countries have repealed or revised their HIV criminalisation laws based on a range of reasons – from futility to privacy rights, to recognising up-to-date science, to concerns over the financial, human or public health cost.
We have been making progress. But now we cannot take any of that progress for granted.
This movement belongs to all of us. And together, even with dwindling resources and some formidable enemies, I believe we can still create a world where justice is not just a concept, but a lived reality for every person living with HIV.
Thank you.